Find out more about diseases starting with the letter “K”: Causalgia, Brain cyst, Cluster headache, Tick-borne encephalitis, Kozhevnikov epilepsy, Colloid cyst of the third ventricle, Coma, Compressive myelopathy, Balo concentric sclerosis, Radicular syndrome, Corticobasal degeneration, Craniovertebral anomalies, Craniospinal tumor, Craniopharyngioma, Myasthenia gravis crises, Hemorrhage into the ventricles of the brain.
Depending on the location of the formation, focal symptoms may be present. The diagnosis is made based on data from computed tomography and magnetic resonance imaging of the head or neurosonography (in children). Therapy consists of aspiration and surgical removal of the formation if complications develop or its growth progresses.
General information about pathology
A cyst is a fluid-filled cavity located in the substance of the brain or its membranes. When the pathology is small in size, it has a subclinical course and is diagnosed accidentally during a neuroimaging examination of the head. Since the intracranial space has limited dimensions, with a significant increase in the volume of the formation, intracranial hypertension develops.
The size of the cavity with liquid is largely determined by the compensatory capabilities of the formation and its localization. Due to the pliability of the skull bones in children at an early age, the cyst may not manifest itself for a long time.
The formation can be found in people of different ages, both in infants and in elderly patients. Even if the fluid cavity is congenital, it can make itself felt only by the age of 30-50.
According to generally accepted practice, treatment is prescribed only in the case of a pronounced clinical picture and when complications develop. If the cavity with fluid is frozen or slowly progressing and its volumes are insignificant, a wait-and-see approach is chosen, which involves regular monitoring of the patient.
Treatment
The cyst is treated both surgically and conservatively.
Removal is carried out using the following methods:
- Puncture - the cyst is pierced with a needle through a small gap in the skull, and then the contents are removed.
- Bypass surgery is performed using a special tube, which is inserted and then used to drain the cavity.
- Trepanation is a surgical operation to remove a cyst by opening the skull.
Classification
Classification by location:
- Cerebral (intracerebral). It is formed in areas of dead brain tissue in the internal structures of the brain.
- Arachnoid. It is formed as a result of the accumulation of cerebrospinal fluid in places of adhesions formed as a result of inflammatory processes and in places of their congenital duplication. The advantage is localized in the meninges.
The following types of brain cysts are distinguished separately:
- dermoid;
- colloidal;
- choroid plexus;
- pineal gland.
According to its genesis, a cavity with fluid can be congenital or acquired. In turn, congenital is divided into colloid and dermoid, and due to its formation into post-infectious, post-traumatic, post-stroke and echinococcal.
Etiology and pathogenesis
The causes of a congenital cyst are unfavorable factors that occur during the development of the fetus. These are:
- fetal hypoxia during delivery;
- fetoplacental insufficiency;
- taking a specific group of medications by a pregnant woman;
- Rh conflict between mother and child;
- intrauterine infections.
Factors that provoke the development of a congenital cavity with fluid are drug, alcohol or nicotine addiction of the mother. In this case, the child’s development takes place under conditions of intrauterine intoxication, which negatively affects the brain structures. The causes of the cavity can also be chronic decompensated diseases of the expectant mother.
An acquired cavity with fluid in the head develops as a result of:
- inflammatory diseases (encephalitis, brain abscess, arachnoiditis, meningitis);
- traumatic brain injuries;
- injuries of newborns received during childbirth;
- cerebrovascular accidents (subarachnoid hemorrhage, ischemic stroke, hemorrhagic stroke).
Depending on the etiology, the following types of liquid cavities are distinguished:
- A cyst of iatrogenic origin forms as a complication after brain surgery.
- Parasitic - develops with paragonimiasis, cerebral form of taeniasis and echinococcosis.
A cavity with fluid can also replace cerebral tissue during degenerative and dystrophic processes in the head.
If a cyst is present, there are a number of factors that can trigger its growth. These include obstruction of venous outflow from the skull, strokes and other vascular disorders, as well as head injuries, hydrocephalus, and neuroinfections.
Brain cyst
The growth of the formation at the initial stage is in most cases accompanied by symptoms of intracranial hypertension. Patients constantly complain of nausea, which has nothing to do with food, deterioration in general health and decreased performance, constant cephalalgia and pressure on the eyeballs.
In some cases, the main symptoms include a constant feeling of pulsation in the head, sleep disturbance, mild hearing loss, dizziness, motor dysfunction, fainting and tremors of the limbs. Possible visual impairment, namely double vision, visual hallucinations, deterioration of visual acuity. With high intracranial hypertension, the patient is worried about constant vomiting.
There are cases when the first signs indicating a cavity with fluid are the first occurrence of epileptic paroxysm. Subsequently, epileptic seizures recur. Paroxysms can take the form of focal Jacksonian epilepsy or absence seizures and be of a primary generalized nature.
Compared to general cerebral manifestations, focal symptoms are observed in fewer cases. These may be sensory disorders, monoparesis and hemiparesis, brainstem symptoms. The latter include dysarthria, eye movement disorders, and swallowing disorders.
One of the complications of formation is cyst rupture. In this case, hemorrhage due to rupture of the vessel, compression of the brain, the formation of an epileptogenic focus and occlusive hydrocephalus are possible.
In the congenital form of the cyst, episyndromes and intracranial hypertension are recorded at an early age. Education in the brain can cause the child to develop mental retardation and mental development disorders.
Main symptoms of echinococcosis
The stages are accompanied by asymptomatic and complicated manifestations. The starting stage lasts up to ten years. Then clinical signs appear. The main symptoms of hydatid cysts:
- Skin itching;
- Loss of appetite;
- Obstructive jaundice;
- Heaviness of the right hypochondrium;
- Bitterness in the mouth;
- Chronic renal failure;
- Headache;
- Impaired mobility;
- Neurological disorders;
- Psychoses.
Alveolar echinococcosis is characterized by a fatal outcome.
Types of brain cysts and their symptoms
Arachnoid - occurs in almost 4% of the population. A cavity with fluid can be congenital or acquired. In the latter case, it develops in response to traumatic brain injury. The formation is localized on the surface of the brain in its membranes. The cavity is filled with cerebrospinal fluid.
In most cases, an arachnoid cyst does not make itself felt for quite a long time and is discovered by chance. Severe symptoms appear only if a large amount of fluid accumulates in the cavity. In this case, cerebrospinal fluid is produced by the cells lining the cavity.
With a sharp increase in the volume of the cavity with liquid, it can rupture and, as a result, die.
Colloid cysts are recorded in 15-20% of all cases of formations inside the ventricles of the brain. Most often it is localized above the foramen of Monroe in the anterior region of the 3rd ventricle. Less common in the area of the transparent cerebral septum in the 4th ventricle.
The liquid filling the cavity of the colloid cyst has high viscosity. Patients experience symptoms of hydrocephalus and, with a certain position of the head, a paroxysmal increase in cephalgia is noted.
In rare cases, memory loss, behavioral disorders and weakness in the limbs occur.
Pineal cyst of the pineal gland - according to statistics, 10% of patients have formations of this type that are small in size and do not make themselves felt. Cystic formations are localized in the epiphysis of the brain, in most cases they are no more than 1 cm in size. Otherwise, symptoms appear. When it grows, it can block the entrance to the “plumbing” of the brain and block the circulation of cerebrospinal fluid, causing occlusive hydrocephalus.
Epidermoid or dermoid is a formation that is an anomaly of intrauterine development. In this case, the cells of the baby's future skin and its appendages remain inside the brain. Accordingly, in addition to liquid, elements of the ectoderm are present, namely sebaceous glands and hair follicles.
After the birth of a child, such a cyst quickly increases in size. The only possible treatment is surgical removal of the formation.
Choroid plexus cyst - forms regardless of the person’s age. In this case, the space between the plexus vessels is filled with cerebrospinal fluid. Symptoms are rarely present, sometimes accompanied by epileptic seizures and symptoms of intracranial hypertension.
With a congenital choroid plexus cyst, the formation is diagnosed at the 20th week of intrauterine development using ultrasound. By the 28th week, such formations resolve.
2. Symptoms of a tumor cyst
Clinically, these neoplasms begin to manifest themselves when pressure comes on the surrounding brain tissue due to the increased size of the cyst. These symptoms are characteristic not only of cysts, but also of other types of benign tumors:
- auditory, visual and olfactory disorders;
- movement coordination disorders;
- inability to concentrate;
- difficulties with memory and speech;
- dizziness, nausea, vomiting;
- partial or complete paresis of the facial muscles;
- loss of sensation in the limbs, convulsions.
Visit our Neurosurgery page
Diagnostic measures
A neurologist may suspect the presence of an intracranial formation of significant size based on the patient’s neurological status and clinical symptoms. In this case, the patient is sent for examination to an ophthalmologist and otolaryngologist to check vision and hearing. Specialists perform ophthalmoscopy, audiometry, perimetry and visometry. With severe hydrocephalus, ophthalmoscopy reveals congested optic discs.
By referring the patient for echo-encephalography, it is possible to diagnose increased intracranial pressure. If the patient experiences epileptic paroxysms, he is additionally sent for electroencephalography.
It is extremely important to differentiate a cavity with fluid from a tumor, abscess and hematoma. It is not possible to do this on the basis of collected clinical data alone. Therefore, to make a clear diagnosis, neurologists use neuroimaging diagnostic methods.
By performing an ultrasound examination, it is possible to diagnose certain types of congenital cysts even at the stage of intrauterine development of the fetus. After birth, until the baby's large fontanelle closes, neurosonography is performed to make the correct diagnosis. In adulthood, to visualize a brain cyst, the patient is sent to a magnetic resonance or computed tomography scan of the head.
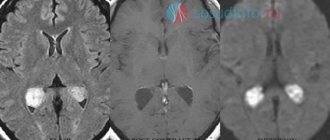
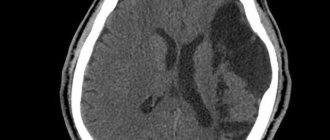
MRI and CT are performed with contrast in order to differentiate a cyst from a tumor. A cavity with liquid is not able to accumulate a contrast agent, unlike a tumor.
After diagnosis, constant monitoring of the patient with a cystic formation is important. During regular examinations, the doctor monitors the volume of the cyst over time.
If the cyst is a consequence of a stroke, additional vascular examinations are carried out: ultrasound, MRI and CT of vessels, duplex scanning.
Diagnostics
The disease can be diagnosed using magnetic resonance imaging .
To detect the causes of a cyst, you must:
- Doppler examination to view the blood vessels of the brain.
- Examine the heart for evidence of heart failure.
- Examine your blood to find out your blood cholesterol levels and do a blood clotting test.
- Determine blood pressure.
- Examine blood for the presence of infections.
- Monitor the rate of cyst growth.
After undergoing a whole range of diagnostic tests, the doctor makes an accurate diagnosis and prescribes treatment for the disease.
General principles of therapy
Drug therapy for cystic formations has practically no results. The only possible treatment is surgical removal of the fluid cavity. But, most forms are small in size and remain in a “dormant” state for many years. In this case, no methods of therapy are used; a wait-and-see regimen is chosen and the patient is regularly examined.
Formations that are accompanied by symptoms of hydrocephalus, complicated by bleeding and rupture, compressing the brain and rapidly increasing in size must be removed. Only a neurosurgeon decides which method of surgical treatment to use.
If the patient has a disorder of consciousness (coma or stupor), he is urgently referred to external ventricular drainage. This method allows you to reduce compression of the brain by the cyst and intracranial pressure. If the cyst ruptures or hemorrhages, surgery is performed. The patient undergoes craniotomy and the formation is excised.
In the absence of complications and disturbances of consciousness, the operation is performed planned and endoscopically. The advantage is the patient’s quick recovery period and low trauma. With endoscopic access, a milling hole is made in the skull, through which fluid is sucked out from the cavity. In order to avoid subsequent accumulation of fluid, several holes are made in the cavity (connected to the cerebrospinal fluid space) or cystoperiotoneal shunting is performed (a special shunt is installed).
The postoperative period involves rehabilitation therapy, including exercise therapy, reflexology and massage. The patient is prescribed drugs to improve blood supply to the brain, absorbents and decongestants.
Differential diagnosis
- CSF collections such as arachnoid cyst and mega cisterna magna are less lobular
- have signal characteristics identical to cerebrospinal fluid on all pulse sequences, incl. FLAIR and DWI
- contain fat
- smaller in size, but can be multiple
- usually a contrast-accumulating solid component is detected
Forecasts
In most cases, a frozen cavity with liquid of insignificant size does not bother the patient and does not cause any symptoms. In other cases, with adequate and timely treatment, the outcome is favorable.
In rare cases, patients after surgical removal of a cyst experience a residual moderate-to-severe liquor-hypertensive symptom. If a focal neurological deficit develops, it persists after treatment.
With the removal of the cyst, epileptic paroxysms disappear, but often appear later. This is justified by changes in the operated area of the head, in particular the formed adhesions. Secondary epilepsy is practically uncontrollable by anticonvulsant therapy.
CT
The combination of cellular debris together with the high cholesterol content reduces the density of the epidermoids to approximately 0 HU; thus, epidermoid cysts may be identical in density to the cerebrospinal fluid, and appear the same as arachnoid cysts.
Calcification is uncommon (10-25% of cases); Rarely, an epidermoid cyst may be hyperdense due to bleeding, saponification, or high protein content (“white epidermoids”).
They do not accumulate contrast, and only in very rare cases show accumulation of contrast by the wall.
They can cause bone erosion, and with an intradiploic location they have a pronounced sclerotic rim along the edges of the cyst [2].
Prevention
An acquired cyst most often becomes a consequence of developing inflammatory, vascular, infectious and post-traumatic processes. Therefore, it is absolutely obvious that only correct and timely treatment of any pathologies, including resorption and neuroprotective therapy, can serve as a preventive measure for the development of formations in the brain.
The only measure to prevent congenital cysts is to protect the woman and fetus from exposure to provoking factors. Equally important are correct management of pregnancy and delivery.
Causes of formation of cystic brain lesions
The causes of congenital pathology are caused by a violation of intrauterine brain formation, which is caused by:
- infectious diseases (herpes, toxoplasmosis, etc.);
- intoxication intrauterine exposure (against the background of professional characteristics, smoking, taking drugs, alcohol, teratogens, radiation);
- thermal effects (abuse of baths, saunas, solariums, hot baths, etc.);
- the presence of Morphan syndrome, hypogenesis.
Causes of acquired cyst of the arachnoid intracranial membrane:
- TBI (concussions, bruises);
- consequence of neurosurgical intervention;
- infections (meningococcal, meningoencephalitis, arachnoiditis, etc.);
- hemorrhages, meningeal hematomas.
An arachnoid cyst can also become a consequence of hyperformation of the spinal substance and its accumulation in the membrane.