Types of paroxysmal activity
Paroxysmal states in neurology are the process of an increase in the amplitude of brain activity on the electroencephalogram. An interesting fact is that the amplitude of the waves not only increases sharply, but also does not appear chaotically. In addition to the waves themselves, the source of their origin is also recorded. Sometimes some doctors deliberately narrow paroxysmal activity to epileptic seizures, however, this is not true.
An interesting fact is that a child may have paroxysms as a variant of the norm, since paroxysmal activity of the brain will not be supported by pathological changes in the structures of the brain.
For adults, it makes sense to talk about paroxysms as a pathological process occurring in the cerebral cortex. If we talk about paroxysm, as the most general concept, we can summarize the following: paroxysm is an intensified attack, occurring at the maximum of its tension and repeating a certain number of times.
Thus, the paroxysmal state will have the following characteristics:
- in the cerebral cortex there is an area with excitation processes that prevail over inhibition processes;
- excitation of the cortex is characterized by a sudden onset and an equally unexpected decline in activity;
- When studying brain impulses, a characteristic pattern is noticeable on the electroencephalogram, in which one can trace the waves reaching their highest amplitude.
Taking into account all the characteristics, the phenomenon of paroxysmal states is classified into two large categories - epileptic and non-epileptic.
Epileptic type of activity is manifested in a sick person by typical conditions - seizures that appear from time to time. These are convulsive conditions that occur with a certain frequency, and sometimes repeat one after another.
Epilepsy can be a congenital pathology, but it can also be acquired if a person has suffered a severe traumatic brain injury, suffers from a brain tumor, intoxication, or has experienced conditions of severe ischemia. Epilepsy, in turn, is also divided into convulsive and non-convulsive; the picture of such conditions is very diverse.
The clinical picture of cerebral paroxysms of both epileptic and non-epileptic origin is distinguished by a variety of manifestations, which sometimes leads to diagnostic errors and the prescription of inadequate therapy. It should be remembered that overdiagnosis of epilepsy in the long term can cause no less harm to the patient than missed cases. Most diagnostic errors can be avoided thanks to a careful and detailed collection of anamnestic information, a competent approach to monitoring the patient and an adequate assessment of instrumental examination methods. The case we describe demonstrates the polymorphism of paroxysmal states in childhood.
Clinical case
Patient V. , was admitted to the neurological department of the 3rd City Children's Clinical Hospital in Minsk at the age of 1 year 6 months with complaints of episodic “rolling” of the eyes to the side for several seconds, while at the time of this paroxysm the child had no reaction to treatment or sound stimuli . Similar conditions were noted by the girl’s mother within a week before admission to the hospital. The disease began with 2 episodes during the day, then the number of paroxysms increased to 10–15 times. The mother denied any previous traumatic damage to the central nervous system; The child also had no previous history of traumatic brain injuries, disturbances of consciousness, or paroxysmal states of epileptic or non-epileptic origin.
From the anamnesis: a child from the 2nd pregnancy, first term birth. Delivery was carried out by vacuum extraction at 41 weeks of gestation. The pregnancy proceeded against the background of the threat of termination due to acute respiratory viral infections in the 1st and 2nd trimesters. Birth weight was 3,810 g, length 51 cm. Artificial feeding. The child's development before hospitalization corresponded to the age norm, vaccinations were completed. During the previous period, the child suffered only colds. The mother denied chronic somatic pathology and surgical interventions. Heredity and transfusion history were not burdened, but the girl had an allergic pathology (food allergy to cow's milk protein).
On admission, the somatic status was unremarkable. Physical development is average, disharmonious in weight. Neurological status: the girl is conscious, emotionally labile, adequate in behavior, accessible for examination and age-appropriate contact. The dream, according to the mother, is calm. On the part of the cranial nerves, slight asymmetry of the nasolabial folds was noted. Upper limbs: range of motion and physiological muscle tone. Muscle strength is age appropriate. Muscle trophism without features. There is no hyperkinesis. SPR D=S, revived, reflexogenic zones are not expanded. Abdominal reflexes D=S, medium alertness. Lower limbs: physiological range of motion. Muscle strength is age appropriate. Muscle trophism without features. Muscle tone is closer to physiological, slightly increased. There is no hyperkinesis. Knee reflexes D=S, Achilles reflexes D=S. There are no pathological foot signs. Coordination sphere without features. He has been walking independently since the age of 1 year 1 month, slightly internally rotating the right foot, with a tendency to place weight on the forefoot (episodic benign dystonic reaction of weight bearing on the foot). There are no meningeal symptoms. Pelvic organs without pathology.
On the second day of stay in the department, the number of episodes of eye movement to the side was about 10. The duration of the episodes ranged from 5–10 seconds to several minutes. Episodes of eye aversion were accompanied by mild coordination disorder, which disappeared 5–10 minutes after the end of the oculomotor paroxysm.
A preliminary diagnosis was made: paroxysmal conditions with the presence of episodes of tonic abduction of the eyes towards an unspecified genesis.
Before the examination, in order to reduce the excitability of the central nervous system, the child was prescribed gromecin at a dose of 0.1 g, 1 tablet 2 times a day.
An electroencephalographic (EEG) examination revealed mild diffuse changes with signs of neurophysiological immaturity. No paroxysmal activity was recorded (see Fig. 1). General and biochemical blood tests without pathology.
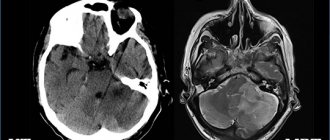
Figure 1. Initial EEG examination. Mild diffuse changes with signs of neurophysiological immaturity. A neuroimaging study (MRI 2 T) revealed signs of a slight increase in the MR signal in the parahippocampal region ( see Fig. 2a ) and a slight expansion of the anterior subarachnoid space ( see Fig. 2b ), which may testify in favor of hypoxic-ischemic perinatal encephalopathy. On the third day, the number of episodes of eye aversion decreased to 6, while their duration did not exceed several seconds.
Figure 2a. MRI study. Signs of increased MR signal in the parahippocampal region.
Figure 2b. MRI study. Signs of a slight expansion of the anterior subarachnoid space. On the fourth day, the number of paroxysms continued to decrease and amounted to only 2 episodes lasting 1–2 seconds. At the same time, no coordination impairments accompanying these conditions were previously noted.
On the fifth day, the episodes of eye aversion completely stopped and did not recur on subsequent days in the hospital.
Repeated EEG examinations carried out on the third and sixth ( see Fig. 3a, 3b ) days from the moment of hospitalization did not reveal regional and pathological forms of bioelectrical activity.
A blood test for viruses, bacteria and protozoa did not reveal a significant infectious factor in the development of the current disease.
Figure 3a. Repeated EEG examination. Mild diffuse changes in the bioelectrical activity of the brain. No regional or pathological forms of activity were identified.
Figure 3b. Repeated EEG examination. Mild diffuse changes in the bioelectrical activity of the brain. No regional or pathological forms of activity were identified.
The final diagnosis: paroxysmal conditions of the type of benign episodes of tonic abduction of the eyes towards non-epileptic origin.
Antiepileptic therapy was not prescribed. The child was discharged home in satisfactory condition.
During a follow-up examination 2 months after discharge from the hospital, it was found that paroxysmal conditions did not recur, and the neurological status remained the same. The girl has advanced in psycho-speech development: her active and passive vocabulary has increased, and she began to speak in two-word sentences. An EEG examination did not reveal any significant changes.
A comment
Benign tonic eye deviations in children are a heterogeneous group of conditions with prolonged episodes of permanent or transient deviations of the eyeballs in the opposite direction to the desired direction with a rapid return to the original position.
The etiology of the described paroxysmal condition is heterogeneous, and the pathogenesis remains not fully established to this day. According to the results of studies by some authors, the disease can have an autosomal recessive and autosomal dominant nature of inheritance. Such patients may have mutations in the calcium channel gene CACNA1A. It is impossible to exclude the possibility of the functional genesis of benign tonic abduction of the eyes to the side due to the immaturity of brain structures and disruption of interneuronal communication.
Most often, researchers consider the hypothesis of age-dependent dysfunction of supranuclear pathways. The etiological factors of symptomatic forms of the disease can be damage to the mesencephalic region - malformation of the vein of Galen, pinealoma, hydrocephalus, pituitary tumor. The iatrogenic nature of this paroxysmal state is also possible. A number of authors indicate its more frequent development in those children whose mothers took valproic acid drugs during pregnancy.
Clinical manifestations of benign tonic eye abduction to the side are somewhat varied. The onset of the disease usually occurs at the age of 4–10 months. In the largest study of this pathology, the age of onset varied from 1 week to 26 months of life (average 5.5 months). The frequency of attacks varies throughout the day from single to hourly. Characteristic is the increase in frequency and severity of paroxysms in infectious diseases accompanied by fever, as well as in physical and psycho-emotional fatigue. As a rule, during the entire period of the disease, no modification of the type of paroxysms occurs. It is believed that the duration of the disease and the time to achieve remission (spontaneous disappearance of the abduction of the eyes) on average can vary from several days to 5 years.
With benign tonic abduction of the eyes to the side and upward, a number of children experience episodes of additional downward tilt of the chin, but a number of authors believe that this is a compensatory mechanism to correct the incorrect position of the eyeballs. With the existing stereotype of moving the eyes in a certain direction, the opposite movement is usually not changed. However, in some patients, unidirectional nystagmus with a fast component in the opposite direction may occur during paroxysm.
In addition, some researchers have described hypometric saccades and divergent strabismus, which can persist for some time (in some cases for a long time) after the cessation of tonic abduction of the eyes.
The described non-epileptic paroxysmal state is periodically accompanied by motor clumsiness and ataxia of varying severity, lasting from several hours to several days. Mild coordination dysfunction may also tend to persist after resolution of the underlying disease.
According to various authors, about 50% of children with benign tonic abduction of the eyes to the side have normal mental development, approximately 40% have a mild intellectual deficit, 10% have moderate to severe intellectual impairment. In the vast majority of cases, normal psychoneurological status in patients with the described variant of paroxysms correlates with spontaneous remission within 2 years from the onset of the disease. If there is a combination of this condition and a neurological and/or cognitive-mnestic deficit, then an additional examination of the child is necessary for the symptomatic nature of the etiology of the pathological process.
Instrumental diagnostic and laboratory studies most often demonstrate normal neuroimaging, electroencephalography and metabolic parameters of blood and cerebrospinal fluid in children with idiopathic (genetic) forms of the disease. The gold standard for neuroimaging examination, MRI of the brain, usually does not reveal pathological changes.
The differential diagnosis of benign tonic eye deviations to the side is carried out with epileptic paroxysmal conditions, in particular with oculomotor seizures and atypical absences.
Specific treatment for this condition has not been developed; attempts at therapeutic intervention are most often ineffective. According to the largest study, therapy with anticonvulsants, acetazolamide and adrenocorticotropic hormone had no effect on the course of the disease. Nevertheless, a number of authors indicate the achievement of a positive effect in relation to the frequency and severity of paroxysms with the use of dihydroxyphenylalanine (levodopa).
Paroxysmal syndrome
In order to understand the essence of this diagnosis, you need to understand some terms. By paroxysm, or attack, we mean a transient dysfunction of any system or organ that occurs suddenly. This condition is divided into two main types: epileptic and non-epileptic.
But speaking generally, we are talking about a situation where a certain painful attack sharply intensifies to the highest degree. In some cases, the term “paroxysmal state” is used to describe recurrent symptoms of a specific disease. We are talking about health problems such as swamp fever, gout, etc.
In fact, paroxysms are a reflection of emerging dysfunction of the autonomic nervous system. The most common causes of such attacks are neuroses, hypothalamic disorders and organic brain damage. Crises may be accompanied by migraines and attacks of temporal lobe epilepsy, as well as severe allergies.
Despite the fact that there are several forms through which the paroxysmal state manifests itself, symptoms with similar characteristics can be found in all cases. We are talking about the following signs: stereotypicality and tendency to regular relapses, reversibility of disorders and short duration. Regardless of the background of what disease the paroxysm made itself felt, these symptoms will be present in any case.
Paroxysmal tachycardia
The question of treatment tactics for patients with paroxysmal tachycardia is decided taking into account the form of arrhythmia (atrial, atrioventricular, ventricular), its etiology, frequency and duration of attacks, the presence or absence of complications during paroxysms (heart or cardiovascular failure).
Most cases of ventricular paroxysmal tachycardia require emergency hospitalization. The exception is idiopathic variants with a benign course and the possibility of rapid relief by administering a certain antiarrhythmic drug. In case of paroxysm of supraventricular tachycardia, patients are hospitalized in the cardiology department in case of development of acute cardiac or cardiovascular failure.
Planned hospitalization of patients with paroxysmal tachycardia is carried out in case of frequent, > 2 times a month, attacks of tachycardia to conduct an in-depth examination, determine treatment tactics and indications for surgical treatment.
The occurrence of an attack of paroxysmal tachycardia requires emergency measures on the spot, and in case of primary paroxysm or concomitant cardiac pathology, a simultaneous call to the emergency cardiological service is necessary.
To relieve paroxysm of tachycardia, they resort to vagal maneuvers - techniques that have a mechanical effect on the vagus nerve. Vagal maneuvers include straining; Valsalva maneuver (an attempt to vigorously exhale with the nasal cleft and oral cavity closed); Aschner's test (uniform and moderate pressure on the upper inner corner of the eyeball); Chermak-Hering test (pressure on the area of one or both carotid sinuses in the area of the carotid artery); an attempt to induce a gag reflex by irritating the root of the tongue; rubbing with cold water, etc. With the help of vagal maneuvers it is possible to stop only attacks of supraventricular paroxysms of tachycardia, but not in all cases. Therefore, the main type of assistance for developing paroxysmal tachycardia is the administration of antiarrhythmic drugs.
As an emergency treatment, intravenous administration of universal antiarrhythmics is indicated, effective for any form of paroxysms: novocainamide, propranoloa (obsidan), ajmaline (gilurythmal), quinidine, rhythmodan (disopyramide, rhythmileka), ethmosin, isoptin, cordarone. For prolonged paroxysms of tachycardia that cannot be controlled by medications, electrical pulse therapy is used.
In the future, patients with paroxysmal tachycardia are subject to outpatient monitoring by a cardiologist, who determines the volume and regimen of antiarrhythmic therapy. The prescription of anti-relapse antiarrhythmic treatment of tachycardia is determined by the frequency and tolerability of attacks. Continuous anti-relapse therapy is indicated for patients with paroxysms of tachycardia that occur 2 or more times a month and require medical assistance to stop them; with more rare but prolonged paroxysms, complicated by the development of acute left ventricular or cardiovascular failure. In patients with frequent, short attacks of supraventricular tachycardia, self-limiting or with the help of vagal maneuvers, the indications for anti-relapse therapy are questionable.
Long-term anti-relapse therapy of paroxysmal tachycardia is carried out with antiarrhythmic drugs (quinidine bisulfate, disopyramide, moracizine, etacizine, amiodarone, verapamil, etc.), as well as cardiac glycosides (digoxin, lanatoside). The selection of the drug and dosage is carried out under electrocardiographic control and monitoring the patient’s well-being.
The use of β-blockers for the treatment of paroxysmal tachycardia can reduce the likelihood of the transition of the ventricular form to ventricular fibrillation. The most effective use of β-blockers in combination with antiarrhythmic drugs, which allows you to reduce the dose of each drug without compromising the effectiveness of the therapy. Prevention of relapses of supraventricular paroxysms of tachycardia, reducing the frequency, duration and severity of their course is achieved by constant oral administration of cardiac glycosides.
Surgical treatment is resorted to in particularly severe cases of paroxysmal tachycardia and ineffectiveness of anti-relapse therapy. As a surgical aid for paroxysms of tachycardia, destruction (mechanical, electrical, laser, chemical, cryogenic) of additional impulse pathways or ectopic foci of automatism, radiofrequency ablation (RFA of the heart), implantation of pacemakers with programmed modes of paired and “capturing” stimulation, or implantation of electrical defibrillators.
Analysis of the rhythm of bioelectric impulses
Biorhythms of the brain are divided into several groups, each of which is named after its Latin letters. So, there are alpha rhythms, beta rhythms, theta and delta rhythms. Depending on the identified rhythm of activity, one can assume what pathology such impulses are associated with.
When deciphering an electroencephalogram, rhythms are the main focus. When reading diagnostic results, it is very important to take into account the symmetry of the appearance of activity in both hemispheres, the basal rhythm, and changes in rhythms during functional loads on the body.
Alpha rhythms normally have an oscillation frequency of 8 to 13 Hertz (Hz). The amplitude of normal oscillations is up to 100 μV. Rhythm pathologies are spoken of in the following cases:
- if the rhythm is associated with neuroses of the third type;
- with interhemispheric asymmetry of more than a third, there is reason to talk about a tumor or cystic neoplasm, a post-stroke condition with tissue scarring, or a previously suffered hemorrhage in this location;
- if the rhythm is unstable, doctors suspect a concussion.
Amplitude disturbances are also recognized as a sign of pathology. Although officially it is the maximum possible 100 μV, but with a value less than 20 and more than 90 units, doctors already suspect pathological abnormalities.
Beta rhythms are also present during normal brain activity and, under certain parameters, do not at all indicate a paroxysmal state. This rhythm is most pronounced in the frontal lobes of the brain.
The amplitude is normally small - from 3 to 5 μV. A normal reserve is an increase in activity by 50 percent, i.e. Even with an amplitude of 7 µV, beta rhythms can be conditionally considered normal, but already when this figure is exceeded they are classified as paroxysmal activity.
For example, waves of this type of diffuse nature with a length of up to 50 µV indicate a concussion. Short spindle-shaped waves will indicate the presence of encephalitis - an inflammatory disease of the meninges, and the frequency and duration of the wave’s existence illustrate the severity of the inflammatory process.
When beta-active waves with a high amplitude of about 30-40 μV and a frequency of about 16-18 Hz are detected in a child, they speak of delays in the child’s mental development.
Theta and delta waves are predominantly recorded in humans during sleep. Therefore, when examined by a doctor while awake, they are not normally recorded. If such waves appear, then this indicates degenerative processes in the brain.
A paroxysmal state usually occurs when the brain matter is compressed, so the doctor may suspect swelling of the brain or a tumor. Theta and delta waves differ in that they indicate severe and profound changes in the brain. Like all waves, theta and delta waves before the age of 21 are not considered a pathology, since in children and adolescents they are a variant of the norm.
In people older than this age, the presence of such waves indicates acquired dementia. In parallel, this is confirmed by synchronous flashes of theta waves with high amplitude. In addition, such waves indicate the presence of neurosis.
Parasomnias
Home → Adult department → Sleep laboratory → Basic sleep disorders → Parasomnias
Parasomnias are various episodic events that occur during sleep. They are numerous, varied and always unexpected in their clinical manifestations. Parasomnias can cause insomnia or drowsiness, psycho-social stress, and harm to self and others. In some cases, parasomnias are a “mask” of a neurological, psychiatric or general somatic disease.
Currently, the Classification of the American Academy of Sleep Medicine (2005) is used to classify sleep disorders, based on which parasomnias are divided into 3 groups: A. Arousal disorders B. Parasomnias associated with FBS C. Other parasomnias
Awakening disorders
combine the options that are most often encountered in clinical practice.
Sleepwalking
(somnambulism, sleepwalking) - is a series of complex motor actions performed by a person in a dream, without awareness of what is happening. According to some data, sleepwalking occurs in 15% of the population. The ratio of occurrence by gender is 1:1. They are most often observed at the age of 4-12 years and, most often, go away on their own with puberty. Usually the patient sits up in bed (and sometimes this is all that ends), then gets up and walks around the room or goes outside the room. “Somnambulists” may perform simple repetitive movements (such as rubbing their eyes, feeling their clothes), but can perform complex creative acts (such as drawing or playing the piano). To an outside observer, “somnambulists” seem strange, with an “absent” facial expression and wide-open eyes. The “somnambulist” is not aware of the danger, which creates a potential threat both for the patient and for the people around him. As a rule, sleepwalking ends spontaneously, continuing with normal sleep, and the patient can return to his bed or fall asleep in any other place. During sleepwalking, sleep talking may occur. During an episode of sleepwalking, a person usually does not perceive anything, and it is very difficult to awaken him. Upon awakening, the “somnambulist” may be confused or even frightened. Typically, an episode of sleepwalking is accompanied by amnesia. Episodes of sleepwalking can occur several times a week or only with predisposing (provoking) factors.
Predisposing factors
. Predisposing factors are: nervous excitement, lack of sleep, external stimuli (noise), internal stimuli (instability of blood pressure, others), drinking alcohol before bed, psychotropic drugs (neuroleptics, antidepressants), drugs.
Causes
sleepwalking. A number of authors believe that the reason for sleepwalking in childhood is brain immaturity. Research also confirms the role of the hereditary-genetic factor in sleepwalking. In adults, sleepwalking often depends on psychological factors and occurs after acute stress or after globally significant life events, often positive.
Night terrors
(sleep terror) are characterized by a sudden onset of screaming, accompanied by motor and behavioral manifestations of intense fear. Tachycardia, tachypnea, hyperhidrosis, mydriasis, decreased skin resistance, and increased muscle tone are observed. The episode may be accompanied by incoherent vocalizations. More often, a person sits up in bed and screams with his eyes open, but not accessible to contact. The episode of night terrors, ending, turns into sleep, and if the person wakes up, he is confused and disoriented. After the end, this episode is amnesic. During an episode of night terrors, the patient may become aggressive, which is dangerous both for himself and for others. Night terrors occur more often in children between 4 and 12 years of age and less often in adults (between 20 and 30 years of age), and are also more common in men.
Predisposing factors
night fears are similar to those during sleepwalking. It has been suggested that the cause of NS is related to brain disorders caused by magnesium deficiency. The prognosis for night fears in children is considered favorable, since with age, episodes of night fears become increasingly rare and completely disappear during puberty.
Sleepy intoxication
(awakening with confused consciousness) is represented by a confused state during the period of awakening and some time after it, manifests itself in a slow transition from sleep to active wakefulness after awakening and is accompanied by various kinds of automatisms with some inhibition of the subject and confusion of consciousness (impaired orientation in space and time) . It is often observed in children who sleep deeply and for long periods of time and is especially often combined with somnambulism, nocturnal enuresis and night terrors.
In the population it occurs in 17.3%, in adults over 15 years old - in 2.9-4.2%.
Behavior can be resistant, or agitated, aggressive and inappropriate to the situation, for example, a person picks up a lamp to talk on it, as if on a telephone, if at that time he is convinced that the phone was ringing. The duration of an episode of sleepy intoxication can be from several minutes to an hour. They are more common in children from 1 to 5 years of age, then their frequency decreases; in adults they are usually associated only with provoking factors. Men and women suffer equally.
A variation of this variant of parasomnia is sleep-related abnormal sexual behavior (sexsomnia), which can manifest itself in the form of prolonged masturbation, sexual activity and aggression, and prolonged sexual sounds.
Among the provoking factors
noted: young age, sleep deprivation, circadian cycle disorders, medications (especially psychotropic). The prognosis is generally favorable.
Treatment of awakening disorders
In most cases, drug treatment is not required. In children, necessary therapy may include: recommendations for sleep hygiene, abstinence from irritants, herbal medicine, phototherapy, psychotherapy, as well as behavioral therapy carried out with parents.
Long-term, frequently recurring episodes of somnambulism are a reason for prescribing drug therapy.
In adults, chronic episodes of arousal disturbances may require psychiatric evaluation and treatment.
Disorders commonly associated with FBS
Nightmares
- fear attacks, anxiety during FMS, which should not be confused with disorders associated with FMS, called night terrors. A nightmare is a long, complex dream that becomes more and more frightening towards the end. The duration and fabulousness (ghostliness) of a dream is a cardinal clinical feature of nightmares. Elements of fear and anxiety are an essential feature of nightmares. At the end of an episode of nightmares, the person quickly comes to a clear consciousness, without confusion. A person remembers the frightening content of a dream well upon awakening, which is a distinctive feature of nightmares. The emotional-affective reaction is usually accompanied by moderate vegetative manifestations. The content of dreams in children almost always poses a danger to the child himself. Nightmares are a common event in children. It should be noted that nightmares can occur while taking psychostimulants, L-DOPA, and barbiturate withdrawal. Rarely disturbing nightmares are common in the population and do not require medication. In cases where nightmares occur frequently, they require psychotherapeutic and psychopharmacological assistance.
Behavioral disorders associated with FBS
- complex motor activity in the FBS associated with the theme of the dream. Motor phenomenology can be elementary (movement of the hand) and very complex, reminiscent of sleepwalking, with sleep-talking, screams, etc. There are idiopathic behavioral disorders associated with FBS (60%), with onset at 60-70 years of age, and symptomatic, with onset at any age with neurological disorders such as dementia, subarachnoid hemorrhage, ischemic cerebrovascular disease, olivo-ponto-cerebellar degeneration, tumor brain Predominant in men.
Sleep paralysis
- a period of inability to perform voluntary movements when falling asleep or waking up. At the same time, eye movements and breathing movements are preserved. These conditions are frightening for the patient, and a feeling of anxiety arises. The duration of the episode is several minutes; completion can occur spontaneously or with external stimulation. Sleep paralysis can occur in isolated form in otherwise healthy people (a familial form that is passed on genetically), and as one of the symptoms of narcolepsy. Sleep paralysis occurs at least once in a lifetime in 40-50% of people. Occasional cases of sleep paralysis are reported in 3-6% of people. In the isolated form of sleep paralysis, treatment is not required. When combined with symptoms of other diseases (usually neurotic disorders), psychopharmacocorrection and psychotherapeutic influence are required.
The section “other parasomnias” includes those options that cannot be classified in the previous sections.
Sleep-related eating disorder
- consists of repeated involuntary, uncontrollable episodes of eating and drinking upon awakening in the middle of the night. As a rule, episodes relate to a state of incomplete awakening, are partially or completely amnesic, and less often are recalled in detail. It is difficult to awaken the patient at such times, and trying to stop him during an eating episode may provoke resistance and anger. Most patients with sleep eating disorders experience episodes almost every night, sometimes several times a night. Eating occurs even in the absence of hunger or thirst. Food is usually eaten very quickly. The entire episode can take no more than 10 minutes and includes the time of getting out of bed, going to the kitchen, and returning to bed.
During episodes, patients tend to consume higher calorie foods, often thicker and sweeter foods, often not their favorite foods during the day. Possible ingestion of strange combinations or types of foods, such as raw meat, buttered cigarettes, or ground coffee; eating or drinking toxic substances, such as cleaning solutions, or foods to which you are allergic. During the episode, the patient may suffer trauma (cuts and burns). In the morning, a person may find real devastation in the kitchen, which helps to remember the details of the episode. In most cases, the problem is protracted, accompanied by depressive disorders and rarely goes away on its own. Other associated problems include loss of appetite in the morning, gastralgia, hypercholesterolemia, and obesity. Many patients with this pathology begin to strictly follow a diet and give themselves intense physical activity during the daytime in order to lose weight.
This pathology most often occurs in women (65-80%) aged 22 to 29 years. Eating disorders during sleep can occur without obvious reasons or under the influence of certain provoking factors: the use of a number of medications; smoking cessation period; period of cessation of alcohol or drug abuse; stress; dieting throughout the day; daytime eating disorders; insomnia, narcolepsy; hepatitis; encephalitis.
Sleepy enuresis
- characterized by repeated involuntary loss of urine that occurs during sleep. The frequency of episodes can range from once a week to nightly and several times a night.
There are primary and secondary enuresis. Primary (idiopathic) enuresis begins at an early age and is likely due to a combination of reasons, among which genetic factors, brain immaturity, signs of dysfunction of the activating ascending systems of the brain, as well as neurotic disorders are of some importance. Secondary enuresis (i.e., involuntary urination at night, which resumes several years after its cessation in early childhood) can be caused by a number of diseases of the urogenital tract, diabetes mellitus, and sickle cell anemia. Often found in the history of patients with epilepsy.
It is believed that at the age of 3 years a child is already able to control the functions of the bladder. The approximate incidence of nocturnal enuresis at the age of 14 years is 22%, in children with mental retardation - 80-90%. Its prevalence decreases by 14-16% between the ages of 5 and 19 years. At the age of 4, sleepy enuresis occurs in 30%, at 6 years - in 10%, at 10 years - in 5%, at 12 years - in 3%, at 18 years - in 1-3% of the population. Primary sleep enuresis occurs in 60-70% of cases and is rare in adults. Sleepy enuresis is more common in boys; at the age of 5 years, the gender ratio is 3:2. Night sleep in children suffering from enuresis is very deep.
In all cases of NE, it is necessary to conduct appropriate clinical and laboratory studies to establish its form and possible etiology.
NE therapy usually consists of a set of measures:
- Regular activities;
- Diet with limited fluid intake before bedtime (4-6 hours before bedtime);
- Exercise therapy: training the abdominal and detrusor muscles (forced and intermittent urination, stretching the bladder, etc.);
- Behavioral methods (diary keeping, control system, rewards);
- Phytotherapy;
- Psychotherapy;
- Physiotherapy;
- Reflexology;
- Special signaling devices (children over 7 years old);
- Drug therapy.
Sleep-related moaning
- a long-term disease, the clinical manifestations of which can occur every night. The main manifestations of the disorder are sounds (moans), quite loud, made by the patient during sleep. During an episode of moaning during sleep, breathing may slow down. It always ends with a sigh or a “moo.” Moans lasting from a few moments to 40 seconds or more are usually repeated several times throughout the night in series lasting from 2 minutes to 1 hour. The facial expression is usually calm, without signs of suffering or discomfort. Despite its frightening nature, moaning in sleep does not appear to be associated with any emotional experience. When the position changes, the moaning usually stops. The cause of sleep-related moaning remains unknown. In most cases, the patient has amnesia for nighttime moaning and does not complain of sleep disturbances, although morning complaints of hoarseness or sore throat are possible. At the same time, the quality of sleep of a person sleeping in the same room or house may be significantly impaired.
Sleep-related dissociative disorders
- psychogenic emotional and behavioral reactions that occur during sleep. Manifestations of this disorder may occur at one of the following time intervals:
- just before going to bed;
- within a few minutes immediately after waking up.
This disorder occurs quite rarely and is more often observed in people who have been subjected to some form of violence - physical, sexual or verbal. In this situation, the episode is often a reconstruction of a previous episode of violence. Emerging memories of previous violence force the body to participate in this event. The episode can last from a few minutes to an hour or more. Typically, the person has no memory of what happened during the episode.
Unlike other types of parasomnias, dissociative disorders occur in the waking state. Treatment is selected individually for each patient and includes psychopharmacology and psychotherapy.
Sleep-related hallucinations
- these are events imagined by the patient that seem very realistic. Most sleep-related hallucinations are visual, but auditory, tactile, taste, and olfactory hallucinations also occur, and hallucinations involving the sensation of movement are also possible.
Sleep hallucinations usually occur: when going to sleep (hypnagogic); upon awakening (hypnopompic). Hallucinations that occur during the daytime may be a sign of narcolepsy.
Complex visual hallucinations in the form of still images of people or animals usually occur after a sudden awakening from sleep. In this case, the person is convinced that he is in a state of wakefulness. Perceived images may have a distorted shape or unusual size. They can remain in the imagination for several minutes. Once the lights in the room are turned on, the hallucinations usually disappear.
Sleep-related hallucinations are quite common. According to a number of researchers, up to one third of people in the general population have reported the presence of such manifestations; sleep-related hallucinations are most often found in children and adolescents. For most people, the frequency of episodes decreases with age. Sleep hallucinations occur in most patients with narcolepsy. Other factors that provoke hallucinations include: taking medications (narcotics) at a given time; past alcohol use; anxiety; disturbances in the emotional sphere; insomnia; epilepsy.
Exploding head syndrome
- a feeling of loud noise in the head that occurs just before going to bed. This noise may sound like a large explosion coming from the head. Similar sensations are possible when waking up during the night. The following are examples of definitions that patients use to describe these sensations: a painless loud bang; the sound of a cymbal (musical instrument); Detonation of bomb.
This condition can cause a person to feel fear and suspect that he has a dangerous disease (for example, a stroke). Frequent and severe episodes can lead to sleep disturbances. Some patients report experiencing flashes of bright colors and muscle twitches in addition to the loud noise. The sensations are usually painless, and painful attacks are rare.
The causes of exploding head syndrome are unknown. This condition can occur in healthy people, more often when overworked and under stress. Treatment includes the prescription of sedatives and psychotherapy.
Parasomnias caused by taking a psychotropic or other biologically active substance
may manifest themselves in the form of parasomnias that occur for the first time, intensification or reactivation of existing parasomnias. In this group, awakening disorders, sleep-related eating disorders, FBS behavior disorder, and sleep-related hallucinations are more common than others.
By definition, this sleep problem occurs only in people who take narcotics or psychotropic medications, and may be considered a side effect of the drug.
Parasomnias associated with any other disease.
Examples of diseases of the internal organs and nervous system that cause these sleep disorders can be: Parkinson's disease; dementia with Lewy bodies; epilepsy; migraine; narcolepsy; brain tumors; mental pathology.
Diagnosis and differential diagnosis of parasomnias is impossible without polysomnography with parallel video monitoring. The most important thing in the differential diagnosis of the causes of parasomnias is to identify the epileptic nature of this phenomenon, which is possible during nighttime VEEG monitoring. If parasomnias do not interfere with social adaptation, patients do not need therapy. At the same time, it is necessary to use both drug and non-drug therapy (psychotherapy, behavioral therapy, acupuncture, phototherapy). The special importance of parasomnias that first appear in adults should also be emphasized, since they are usually secondary and are masks for other diseases. The universal rule for the treatment of parasomnias is to maintain a constant sleep pattern.
ME AND. Levin. Parasomnias – the current state of the problem //Epilepsy. – 2010, N2, p.10-16.
Provoking factors
So, understanding that the basis of such a problem as a paroxysmal state is in fact always cerebral disorders, it is worth paying attention to those diseases that can lead to a sudden deterioration in physical condition, without the appearance of noticeable symptoms before.
It is this fact that allows us to assert that with all the abundance of various pathologies that serve as the background for a crisis, it is almost always possible to trace a single etiological picture.
You need to understand that doctors pay enough attention to this problem, so a study was carried out on the condition of a significant number of patients in order to identify common etiological factors that lead to the occurrence of paroxysms. The examinations were focused primarily on working with diseases such as vegetative-vascular dystonia, migraine, epilepsy, neuralgia and neuroses, etc.
What diseases lead to a crisis?
- Some hereditary diseases actively provoke the appearance of central paroxysms. Of these, the most common are systemic degenerations of the central nervous system (Wilson-Konovalov disease, Tourette's disease), metabolic diseases caused by heredity (phenylketonuria, Gaucher disease, leukodystrophies, glycogenosis, galactosemia), a group of epileptic diseases and others.
- Organic diseases of the nervous system. In the first row are traumatic brain injuries, post-traumatic cerebrovascular diseases, and causalgia. Neoplasms in the brain and spinal cord, vascular pathologies of brain networks, strokes, ischemic diseases, neuralgia of the trigeminal, glossopharyngeal and upper laryngeal nerves.
- The manifestation of paroxysms is characteristic of a number of diseases of the psychovegetative syndrome: vegetative-vascular pathologies, Charlen's syndrome, Slader's syndrome, neuroses, migraines, depressive states, hysteria, affective disorders.
- Paroxysmal conditions in certain diseases of internal organs - congenital heart defects, myocardial infarction, renal failure, uremia, acute hepatitis, hepatic coma, pneumonia, bronchial asthma, malignant lung diseases, blood diseases.
- Diseases of the endocrine system and metabolic disorders - pheochromocytoma, Cushing's disease, menopausal syndrome, hypoxia, hypercapnia;
- Paroxysms are characteristic of a whole range of infectious encephalitis, neurosyphilis, complications after vaccination, parasitic infestations (cysticercosis, echinococcosis).
- They often provoke a paroxysmal state of intoxication due to alcohol and drug poisoning, long-term use of certain medications, and technical poisoning.
Migraine-like paroxysms
Headaches are one of the most common signs of cerebral pathologies. Several main etiological causes contributing to the occurrence of headache have been identified: vascular disorders, muscle tension, liquorodynamic causes, neuralgic etiology, mixed and central.
Each etiological factor is characterized by a separate mechanism for the occurrence of pain, but the basis is always a dysfunction of the nerve cells of the brain. In particular, migraine is characterized by vascular disorders, when high or low blood pressure in the network of cerebral capillaries provides regular insufficient trophism of neurons, or pressure from dilated blood vessels occurs on brain tissue.
Paroxysms during migraine belong to the non-epileptic series and are expressed in the form of regular attacks of pain in the area of one side of the head. The pain is excruciating and very long-lasting, sometimes lasting for several days. A feature of migraine-like paroxysms is their sufficient resistance to treatment - it can be extremely difficult to stop the pain.
An extraordinary feature of migraine is the fact that the paroxysmal state in this pathology can be both a clinical sign and also join the complex of symptoms of other cerebral pathologies. This situation makes it much more difficult to make a correct diagnosis - it is extremely difficult to discern third-party diseases behind migraine attacks.
Diseases with characteristic manifestations of paroxysm
As mentioned above, in the vast majority of cases, a sharp exacerbation of symptoms occurs due to dysfunction of the brain. In addition, manifestations that are directly related to cerebral disorders are often recorded, and this is one of the key features of this condition.
In addition, you need to understand that there are both primary and secondary paroxysmal genesis. Primary is caused exclusively by congenital factors of manifestation, such as disorders in the brain and genetic disposition, which is formed during the development of the embryo. Secondary paroxysm is a consequence of the influence of internal and external factors. It manifests itself already during life.
The peculiarities of such a problem do not end there. Such paroxysmal states are recorded in neurology, which accompany the disease throughout the entire period of its course. Also, a sharp increase in symptoms may be one-time in nature and result from a state of shock in the central nervous system. One striking example is acute blood loss or a sudden increase in temperature.
Panic disorder (episodic paroxysmal anxiety)
To treat paroxysmal conditions, consultation with a neurologist is necessary. Before prescribing treatment, the neurologist must know exactly the type of attacks and their cause. To diagnose the condition, the doctor clarifies the patient’s medical history: when the first episodes of attacks began, under what circumstances, what their nature is, and whether there are any concomitant diseases. Next, you need to undergo instrumental studies, which may include EEG, EEG video monitoring, MRI of the brain and others.
After performing an in-depth examination and clarifying the diagnosis, the neurologist selects treatment strictly individually for each patient. Therapy for paroxysmal conditions consists of medications in certain doses. Often the dosage and the drugs themselves are selected gradually until the required therapeutic effect is achieved.
Typically, treatment of paroxysmal conditions takes a long period of time. The patient should be constantly monitored by a neurologist for timely adjustment of therapy if necessary. The doctor monitors the patient’s condition, assesses the tolerability of the drugs and the severity of adverse reactions (if any).
The Yusupov Hospital has a staff of professional neurologists who have extensive experience in treating paroxysmal conditions. Doctors are proficient in modern effective methods of treating neurological pathologies, which allows them to achieve great results. The Yusupov Hospital performs diagnostics of any complexity.
The clinic is located near the center of Moscow and receives patients around the clock. You can make an appointment and get advice from specialists by calling the Yusupov Hospital.
Panic disorder is a mental disorder in which the patient experiences spontaneous panic attacks. Panic disorder is also called episodic paroxysmal anxiety disorder. Panic attacks can occur from several times a day to once or twice a year, while the person is constantly expecting them. Severe anxiety attacks are unpredictable because their occurrence does not depend on the situation or circumstances.
This condition can significantly impair a person's quality of life. The feeling of panic can be repeated several times a day and last for an hour. Paroxysmal anxiety can occur suddenly and cannot be controlled. As a result, a person will feel discomfort while in society.
The manifestations of paroxysmal sleep disorders are very diverse. These may include:
- nightmares;
- talking and screaming in sleep;
- sleepwalking;
- motor activity;
- night cramps;
- shuddering when falling asleep.
Paroxysmal sleep disorders do not allow the patient to regain strength or rest properly. After waking up, a person may feel headaches, fatigue and weakness. Sleep disorders are common in patients with epilepsy. People with this diagnosis often have realistic, vivid nightmares in which they run somewhere or fall from a height.
During nightmares, your heart rate may increase and you may perspire. Such dreams are usually remembered and can be repeated over time. In some cases, during sleep disorders, breathing disturbance occurs; a person may hold his breath for a long period of time, and there may be erratic movements of the arms and legs.
Treatment of insomnia in patients with neurotic disorders
E.A. KORABELNIKOVA
, Doctor of Medical Sciences, Professor,
First Moscow State Medical University named after.
I. M. Sechenova The relevance of studying insomnia within the framework of neurotic disorders is due not only to the high frequency of occurrence (65-100%). Traditionally, insomnia is classified as one of the most difficult to tolerate and maladaptive manifestations of neurotic disorders. Insomnia and neurotic state are closely related. On the one hand, sleep disturbances in neurotic disorders can be considered as a typical manifestation in the clinical picture of disorders of the neurotic circle, on the other hand, primary insomnia, with its progression and lack of timely treatment, is often a trigger that causes the addition of other neurotic disorders. In this regard, the treatment of insomnia within the framework of neurotic disorders is carried out in two directions: treatment of the underlying disease and insomnia as the leading syndrome. According to the results of numerous studies, in most cases the most effective treatment is combination treatment, in which drug treatment is combined with psychotherapy.
The problem of neurotic disorders is of great medical and social importance, which is associated with their high prevalence. The term “neurosis” was introduced in 1776 by the Scottish physician W. Cullen to designate “disorders of sensations and movements that are not accompanied by fever and do not depend on local damage to any organ.” With this approach, neuroses often included not only purely “functional” diseases, but also degenerative diseases, metabolic diseases, etc. Later, the concept of “neuroses” was limited to disorders caused or provoked by a traumatic situation. In the International Classification of Diseases, 10th revision (ICD-10), the term “neurosis” is replaced by the term “neurotic disorders.” However, the concept of “neurosis” has not lost its meaning and is widely used both in scientific literature and in practice.
In the modern teaching on neurotic disorders, a tendency is revealed to combine biological, psychological and social mechanisms of etiopathogenesis, considering them in an inextricable dynamic interaction [1, 6, 13]. It is this view of neuroses that makes it possible to consider their specificity in relation to other psychogenic disorders and to develop a differentiated approach to the diagnosis and treatment of neurotic conditions.
To identify neurotic disorders, the principles of positive and negative diagnostics are traditionally used [13]. Within the framework of positive diagnostics, the recognition of neurotic disorders is based on the identification of specific clinical manifestations (symptoms and syndromes) and the psychogenic mechanism of formation. The second diagnostic paradigm is based on the absence of mental disorders of a different level in the clinical picture, as well as the exclusion of neurosis-like and pseudoneurotic disorders of organic, somatic or schizophrenic origin.
One of the currently most common definitions of neurosis was proposed by A. M. Vein (1982), who, along with the significance for the diagnosis of neuroses of the psychogenic factor, personality characteristics, insufficiency of psychological defense and the formation of neurotic conflict, identified specific clinical manifestations, classifying disorders as in the emotional, vegetative and somatic spheres [1].
The clinical picture is polymorphic and includes a variety of symptoms, both paroxysmal and permanent. Among them, sleep disorders come in first place in terms of frequency of occurrence, and according to some researchers they are considered as an obligate symptom of a neurotic disorder. Data from clinical and epidemiological studies show that in neurotic disorders, various forms of sleep disorders occur with a frequency of 65 to 100% [2, 11, 21].
According to the latest 2005 International Classification of Sleep Disorders [16], insomnia is defined as “recurrent disturbances in the initiation, duration, consolidation or quality of sleep, occurring despite the availability of sufficient time and conditions for sleep and manifested by disturbances of various types of daytime activities.” The common everyday term “insomnia” has no physiological meaning (it is impossible to achieve a complete lack of sleep for a long period).
According to the course, insomnia is divided into acute (lasting less than 3 weeks) and chronic (lasting more than 3 weeks). Insomnia lasting less than 1 week is defined as transient.
The clinical phenomenology of isomnia includes presomnia (difficulty falling asleep, fear of not falling asleep), intrasomnia (shallow sleep with frequent awakenings) and post-somnia disorders (problem of early morning awakening, decreased performance, feeling of dissatisfaction with sleep).
Classification of insomnia depending on the mechanism of formation is presented in Table 1
. Patients with neurotic disorders may exhibit various types of insomnia: both specific (group 5) and nonspecific (adaptive, psychophysiological insomnia, pseudo-insomnia, insomnia developing against the background of inadequate sleep hygiene, insomnia associated with taking medications, as well as disorder of biological rhythms).
| Table 1. Classification of insomnia depending on the etiological factor | |
| Variant of insomnia | Characteristic |
| Adaptive (acute) | Occurs against the background of acute stress, conflict or environmental change. Duration - no more than 3 months. |
| Psychophysiological insomnia | Characterized by accompanying psychological disorders, “fear of not falling asleep,” excessive activation and “trying” to fall asleep, leading to worsening sleep disorders. Duration - more than 3 months. |
| Idiopathic insomnia | Diagnosed only when it is impossible to determine the cause of sleep disorders that began in early childhood without an obvious cause and are present throughout the patient's life without significant periods of improvement. |
| Pseudoinsomnia | Characterized by a disturbance in the perception of one’s own sleep (periods of being awake at night are well remembered, and periods of sleep, on the contrary, are amnesic) and fixation on one’s own health problems associated with sleep disturbances |
| Insomnia in mental disorders | Formed as a symptom of a neurotic disorder |
| Insomnia due to inadequate sleep hygiene | Formed as a consequence of the characteristics of human life, which lead to increased activation of the nervous system in the periods preceding bedtime |
| Drug-related insomnia | Develops as a result of inadequate (in dosage or duration) use of medications (most often sleeping pills) |
| Sleep disorders associated with a disorder of biological signals that signal the onset of sleep provide preparation for the onset of sleep either too late or too early | |
The relevance of studying insomnia within the framework of neurotic disorders is due not only to their high frequency of occurrence. Among all the manifestations of neurotic disorders, insomnia is traditionally classified as one of the most difficult subjectively tolerable and maladaptive [4, 6, 15]. Insomnia and a neurotic state are characterized not by one-sided, but, undoubtedly, by two-way connections. On the one hand, sleep disturbances in neurotic disorders can be considered as a typical manifestation in the clinical picture of disorders of the neurotic circle, on the other hand, primary insomnia with its progression and lack of timely treatment, in turn, is often a trigger that causes the addition of other neurotic disorders or another form of mental pathology [3].
That is why the treatment of insomnia within the framework of neurotic disorders is carried out in two directions: treatment of the underlying disease and insomnia as the leading syndrome. According to the results of numerous studies, in most cases the most effective is combination treatment, in which drug treatment is combined with psychotherapy.
The psychopharmacological complex includes a combination of tranquilizers, antidepressants of both herbal origin and psychotropic drugs. The leading method of treatment for neurotic disorders is psychotherapy, mainly multimodal, combining various complementary psychotherapeutic techniques: rational, cognitive, suggestive, behavioral, family, game, art therapy, gestalt therapy, etc. Combinations of these methods depend on the depth of neurotic disorders, the nature neurotic syndrome, type of psychological conflict, individual adaptive pattern, age, personality characteristics and other subjective factors. Selection of an individual treatment regimen is possible only after a thorough examination and is carried out taking into account all the characteristics of the disease.
In the treatment of insomnia as a leading syndrome in neurotic disorders, the leaders so far are tranquilizers - benzodiazepine derivatives, which, unfortunately, themselves create certain problems, such as addiction, dependence, the need to constantly increase the dose of the drug with long-term use, a negative effect on the course of breathing disorders during sleep (for most drugs), somatic complications (allergies, effects on the gastrointestinal tract, etc.). We must not forget that the abuse of sleeping pills in itself contributes to the development of insomnia.
The most modern hypnotics are derivatives of cyclopyrrolone (zopiclone) and imidazopyridine (zolpidem). These drugs, along with a hypnotic effect, have varying degrees of sedative, anxiolytic, anticonvulsant and muscle relaxant effects. The advantages of the drugs include the absence of addiction, physiology, short half-life and, as a result, the absence of disturbances in daytime wakefulness.
An alternative to strong sleeping pills on the modern drug market are non-hypnotic drugs of other pharmacological groups, which also have a hypnotic effect.
Such drugs include, in particular, doxylamine succinate (Donormil). The main point of application for sleeping pills is the GABA-benzodiazepine chloride complex (Costa complex). To date, the heterogeneity of the benzodiazepine receptor has been well studied, and the existence of such subtypes as omega-1, -2, -5 and -6 has been proven. It is known that omega-1 receptor subtypes are distributed predominantly in the cortical and subcortical areas and, accordingly, when interacting with them, a hypnotic effect occurs. Omega-5 and -6 subtypes are located predominantly in the spinal cord and peripheral tissues, and effects such as muscle relaxant and anticonvulsant are associated with their stimulation. Modern drugs (third-generation hypnotics) are distinguished by a pronounced selectivity of neurochemical action to various components of the Costa complex (i.e., they act predominantly on omega-1 receptors). Thus, the main effect of these drugs is the activation of somnogenic systems (7).
The half-life of doxylamine is 10 hours. It is recommended to take one tablet 15-30 minutes before bedtime. Doxylamine succinate is prescribed, as a rule, for 2-5 days.
Treatment of insomnia with doxylamine succinate is effective and safe, as shown in many foreign and domestic studies [5, 7, 12, 20]. In particular, a study of the effect of the drug on healthy volunteers [7] showed that doxylamine succinate leads to a decrease in the duration of night awakenings, a decrease in the duration of the first stage of sleep and an increase in the second without a significant effect on the duration of the third and fourth stages of sleep and the REM phase. There was no significant subjective effect on the reports of healthy volunteers, however, compared with placebo, doxylamine increased the depth of sleep and its quality. The drug did not have a significant effect on short-term memory. The lack of differences in the effects of doxylamine and placebo on levels of consciousness, anxiety and drowsiness is important evidence of its safety in this regard. It should also be noted that no adverse events were reported in this study.
A study of 61 patients with various forms of neurotic disorders accompanied by sleep disorders, conducted in the clinic of the department for the study of borderline mental pathology and psychosomatic disorders of the State Scientific Center for Mental Health of the Russian Academy of Medical Sciences, showed the effectiveness and safety of doxylamine in the treatment of this category of patients [14]. Thus, as a result of treatment, it was revealed that the drug has a positive effect on sleep in general. Thus, in 73.8% of cases, there was a significant improvement in falling asleep, and frightening dreams disappeared. The drug caused a significant improvement in the quality of morning awakening and did not affect the number of night awakenings. All patients in this study reported good tolerability of the drug. Thus, even those unpleasant phenomena that were noted (morning drowsiness and lethargy, difficulties in joining work activities) decreased to insignificant or completely disappeared when the dose was reduced. The drug can be used during pregnancy (instructions for medical use of the drug Donormil). Experimental and clinical studies did not reveal any teratogenic or embryotoxic effects of the drug.
Another group of drugs are low-dose antidepressants for sleep disorders without depression. In patients with depression and insomnia, studies have shown that sedative antidepressants improve sleep [23, 28]. However, quite often antidepressants used in low doses are used as sleeping pills in patients with insomnia without clinically significant depression. The benefit of this approach is that when using these drugs, addiction and physical dependence do not develop.
Sometimes, in the treatment of insomnia, the side sedative effects of certain nootropic drugs, in particular Phenibut, are used, especially in pediatric practice.
In recent years, great interest has been shown in the sleep-inducing properties of melatonin. As a hormone of the pineal gland, it is involved in maintaining normal circadian rhythm in humans. Synthetic analogues of melatonin make it possible to normalize the level of this hormone in the central nervous system. They are quite effective and safe hypnotics that can be recommended in all cases of sleep disorders, in patients of any age and with any concomitant pathology, without any visible negative consequences and with a high degree of tolerability [27].
Other drugs with a hypnotic effect include homeopathic drugs and herbal remedies. One example of an over-the-counter product with a proven positive effect on sleep is the Melisan elixir.
It is preferable to start drug treatment with herbal sleeping pills and homeopathic drugs and melatonin (so-called over-the-counter remedies). If these drugs are ineffective within 3-5 nights, they are replaced with more potent ones - modern sleeping pills with minimal risk of developing drug dependence and addiction (doxylamine, zopiclone, zolpidem, zaleplon). For long-term use as sleeping pills without the risk of developing addiction and dependence, antidepressants with a sedative effect and melatonergic drugs are recommended.
An important and necessary condition for the effectiveness of any therapeutic intervention for sleep disorders is adherence to sleep hygiene [29, 30]. It is recommended to sleep on a wide, firm bed, have a comfortable mattress with a flat surface, darker tones of linen, and comfortable nightwear. Daily exercise is important for maintaining healthy sleep, but can disrupt it if done close to bed. It is important to maintain optimally comfortable temperature and humidity conditions and regulate the degree of noise intensity. It is advisable that the head be open, while the legs are warmly covered. Before going to bed, you should avoid vigorous physical activity, do not overeat or drink large amounts of liquid, caffeine-containing and other stimulant drugs, do not smoke, and do not drink alcohol. You need to go to bed and get up at the same time.
The light pattern of the sleep-wake cycle is extremely important for normal sleep. During the daytime, it is recommended to be in bright light, which stimulates the mechanisms of wakefulness and has a beneficial effect on subsequent sleep. Immediately before bedtime, water treatments are effective. The dynamics of body temperature after taking a bath (increase and subsequent decrease) triggers the body’s circadian rhythm. Baths with substances that have a calming effect are effective: pine needles, sea salt, special bath foam, etc. Another method recommended in the complex treatment of insomnia is aromatherapy [17, 18], which is used in the form of massage with essential oils, inhalations, vapors and aromatic baths, soporific herbal pillows. Acupressure and acupuncture provide a certain effect for insomnia of various origins. Its use is based on the ideas of ancient Eastern physicians about the presence of certain points on the human body, by acting on which one can activate the body’s self-regulation systems. The complex of therapy for sleep disorders often includes individually selected therapeutic music and “natural noises” [8, 19, 31].
Among non-pharmacological methods of treating insomnia in neurotic disorders, the leaders are, of course, various methods of psychotherapy and behavioral psychocorrection. Studies have shown that psychotherapy is no less effective at improving sleep than medications [9, 10, 22, 25, 26, 29]. Pathogenetic methods of psychotherapy for neurotic disorders in this situation are combined with symptomatic methods of psychotherapy for insomnia as a leading syndrome ( Table 2
).
| Table 2. Methods of psychotherapy for insomnia as a leading syndrome | ||
| Group | Methods | Characteristic |
| Rational psychotherapy | Explanatory work Psychotherapeutic mirror | Discussion of the role of sleep in human life, the strength of the brain mechanisms for ensuring it, the unintentional exaggeration by patients of the degree and significance of sleep disorders, the absence of a fatal threat to their life in sleep disorders, treatment prospects. Presentation by a psychotherapist of real case histories of patients suffering from insomnia, psychotherapeutic work with them led to recovery |
| Behavioral psychotherapy | Journaling Ritual Sleep restriction therapy Method "stimulus-control" ("stimulus-regulation") | Daily recording of the patient's subjective impression of sleep and keeping a daily activity log (detailed description of daytime events, physical and emotional factors) A standard, unchanging in time and sequence set of actions preceding sleep Maximizing sleep efficiency by reducing the total time spent in bed to the total time spent sleeping, but not more than 4.5 hours Achieving the ability to quickly fall asleep at a certain time. To do this, it is not recommended to go to bed until drowsiness appears. Patients are taught to associate the sleeping room (or sleeping place in the absence of one) only with sleep |
| Paradoxical psychotherapy | Method of paradoxical intention | Aimed at overcoming anxiety of anticipation. The essence of the influence is to encourage the patient to do something that is contrary to common sense, i.e. not sleep at all |
| Self-regulation methods | Relaxation training, calming exercises (stretching, self-massage), imagination exercises | Influencing sleep by changing the previous state of wakefulness. Reduced muscle and emotional tension |
| Cognitive therapy | Overcoming negative thoughts, an alternative strategy for perceiving the problem | Identifying dysfunctional beliefs and ideas about sleep in patients and replacing them with more adaptive alternatives, i.e. replacing “catastrophizing” thoughts with calmer ones |
Moreover, the effect of drugs on sleep often ceases almost immediately after the end of treatment, while the results of normalization of sleep patterns persist in the future [24].
In addition, psychotherapy does not cause addiction or side effects, which is often observed with the use of sleeping pills. Literature
1. Airapetyants M.G., Vein A.M. Neuroses in experiment and in the clinic. M., 1982. 272 p. 2. Aleksandrovsky Yu.A., Avedisova A.S., Pavlova M.S., Gorinov A.A. Modern psychopharmacotherapy of psychogenic sleep disorders. A manual for doctors. M.: M3 RF, 1998. 3. Androsova V.V. Features of the action of hypnotics in the treatment of sleep disorders in patients with neurotic disorders: dissertation. ...cand. honey. Sci. M., 2004. 113 p. 4. Autonomic disorders. Clinic, diagnosis, treatment. Ed. Veina A. M. Publisher: M.: Medical Information Agency. 752 pp. 5. Vein A.M. Report on studies of Donormil in patients with insomnia. M., 1997. 6. Karvasarsky B. D. Neuroses. 2nd ed., revised. and additional M. Medicine, 1990. 576 p. 7. Kovrov G.V., Machulina A.I., Lyubshina O.V. Prospects for the use of Donormil in the treatment of insomnia. RMJ. 2007. 15. 24: 1788–1794. 8. Korabelnikova E.A. Music and sleep. Sound and music in our lives. Sat. reports of the scientific-practical conference. M., 2010. pp. 25-33. 9. Korabelnikova E.A. Possibilities of treating sleep disorders without the use of sleeping pills. Effective pharmacotherapy. Neurology and psychiatry. Special issue “Sleep and its disorders”, 2013. 12: 30-38. 10. Korabelnikova E.A. Psychotherapy for insomnia: the role of a somnologist and psychotherapist. Effective pharmacotherapy. Neurology and psychiatry. Special issue “Sleep and its disorders”, 2014. 12: 38-44. 11. Levin Ya.I., Vein A.M. The problem of insomnia in general medical practice. Ross. Honey. Zhurn., 1996. 3: 16-19. 12. Levin Ya.I., Strygin K.N. Donormil in the treatment of insomnia. Treatment of nervous diseases, 2005. 6. 2(16): 18-21. 13. Mendelevich V.D., Solovyova S.L. Neurosology and psychosomatic medicine. M.: MEDpress-inform, 2002. 14. Smulevich A.B., Zheleznova M.V., Pavlova L.K. The use of the drug "Donormil" in the treatment of sleep disorders of moderate and mild severity in the practice of a psychiatrist. Psychiatry and psychopharmacotherapy, 2006. 8. 1: 21-28. 15. Shpak V.M. Sleep disorders and their treatment for neuroses and some neurosis-like conditions: Diss. doc. honey. Sci. M., 1968. 16. American Academy of Sleep Medicine. International classification of sleep disorders, 2nd ed.: Diagnostic and Coding Manual. Westchester, Illinois: American Academy of Sleep Medicine, 2005. 17. Buckle J. Clinical Aromatherapy. J. Buckle. 2nd ed. London: Elsevier Limited. 2004. 416 p. 18. Bykov AT et al. Conscious and unconscious sensory inflows allow effectively control the various functions of human organism. Spanish J. of Psychology, 2006. 2: 201–218. 19. Gagner-Tjellesen D, Yurkovich EE, Gragert M. Use of music therapy and other ITNIs in acute care. J. Psychosoc. Nurs. Ment. Health Serv., 2001. 39. 10: 26–37. 20. Hausser-Hauw et al. Effect on sleep architecture and residual effect of a dose of 15 mg of Doxylamine in healthy volunteers. Sep Hop Paris, 1995. 71: 23–24, 742–750. 21. Langer S, Mendelson W. Symptomatic treatment of insomnia. Sleep, 1999. 15(22): 701-704. 22. Lichstein KL, Wilson NM, Johnson CT. Psychological treatment of secondary insomnia. Psychol. Aging., 2000. 15: 232–240. 23. Mendelson WB. A review of the evidence for the efficacy and safety of trazodone in insomnia. J Clin Psychiatry 2005. 66: 469-476. 24. Morin CM et al. Insomnia and chronic use of benzodiazepines: A randomized clinical trial of supervised taperting, cognitive-behavioral therapy, and a combined approach to facilitate benzo-diazepine discontinuation. Am. J Psychiatry 2004 161: 332–342. 25. Morin CM et al. Nonpharmacologic treatment of chronic insomnia. An. Am. Acad. of Sleep Medicine review. Sleep. 1999. 22. 8: 1134–1156. 26. Morin CM, Espie CA. Insomnia: A clinical guide to assessment and treatment. New York: Kluwer Academic/Plenium, 2003. 27. Olde-Rikkert MC, Rigaud AS. Melatonin in elderly patients with insomnia: a systematic review. Z. Gerontol. Geriatr., 2001. 34. 6: 491–497. 28. Roth T, Zorick F, Wittig R, McLenaghan A, Roehrs T. The effects of doxepin HCl on sleep and depression. J Clin Psychiatry 1982. 43: 366-368. 29. Silber MH. Clinical practice. Chronic Insomnia. New England J Med 2005 353 8: 803–810. 30. Stepanski EJ, Wyatt JK. Use of sleep hygiene in the treatment of insomnia. Sleep Med. Rev., 2003. 7: 215–225. 31. Wigram T, Pederson IN., Bonde LO. A comprehensive guide to music therapy: theory, clinical practice, research and training. London: Jessica Kingsley, 2002. 381 p.
Source:
Medical Council, No. 10, 2015
Results of examination of children's condition
When a child is bothered by frequent headaches, the pediatrician refers him to a consultation with a pediatric neurologist. Finding out the cause of pain is not easy, but now there are harmless, reliable and informative methods for examining even the smallest children.
Electroencephalography and echoencephaloscopy are prescribed by specialists for deviations in speech, mental, and motor development. These research methods make it possible to identify many other disorders in the functioning of the central nervous system.
EEG allows you to study brain activity and give an accurate assessment of the child’s development. READ ALSO: what does an MRI of a child’s brain show?
In order to understand what non-epileptic paroxysmal states look like in children, it makes sense to pay attention to several current examples.
First of all, these are short-term breath holdings. This problem can be caused by severe fear, frustration, pain, or any surprise. During this condition, the child may scream, while the scream itself is delayed while exhaling, which is often followed by loss of consciousness.
Attacks of this kind are most often recorded in the age period from 6 months to 3 years. The good news is that their presence does not increase the risk of cognitive decline or epilepsy.
Paroxysmal state in a child - what is it? It is worth paying attention to one more example that clearly demonstrates a similar problem. We are talking about loss of consciousness. Fainting in this case is the result of acute circulatory failure in the brain area. In fact, this is nothing more than a manifestation of vascular lability.
Fainting occurs mainly in adolescents; among children who are at an early age, such conditions are rare. As for the causes of this problem, they include a sharp transition from a horizontal to a vertical position, as well as a state of strong emotional arousal.
Fainting begins with a feeling of darkening in the eyes and dizziness. In this case, both loss of consciousness and loss of muscle tone occur at the same time. There is always a possibility that short-term clonic convulsions may occur during depression of the child’s consciousness. As a rule, children do not remain unconscious due to fainting for more than 1 minute.
Reflex epilepsy is another problem that can be caused by a paroxysmal state in a child. It is unnecessary to say that this is a rather dangerous condition. Stressful situations and flashes of light can provoke such manifestations. But complex activities and auditory stimuli are unlikely to cause reflex epilepsy.
Paroxysmal state in a child - what is it? It is worth paying attention to one more example that clearly demonstrates a similar problem. We are talking about loss of consciousness. Fainting in this case is the result of acute circulatory failure in the brain area. In fact, this is nothing more than a manifestation of vascular lability.
Fainting occurs mainly in adolescents; among children who are at an early age, such conditions are rare. As for the causes of this problem, they include a sharp transition from a horizontal to a vertical position, as well as a state of strong emotional arousal.
Reflex epilepsy is another problem that can be caused by a paroxysmal state in a child. It is unnecessary to say that this is a rather dangerous condition. Stressful situations and flashes of light can provoke such manifestations. But complex activities and auditory stimuli are unlikely to cause reflex epilepsy.
Paroxysmal sleep disorders in children
P. Schwarzmayr, K. Mayer-Ewert
Diagnosis and treatment of epilepsy in children
- M.: Mozhaisk-Terra 1997.-656 p.
INTRODUCTION
Paroxysmal sleep disorders have been known since antiquity, and already in the works of Hypnocrates and Aristotle, some of them were described, both epileptic and non-epilentic conditions observed in sleep. To date, a large number of nosologically independent syndromes accompanied by paroxysmal sleep disturbances are known.
Differential diagnosis of sleep disorder syndromes of epileptic and non-epileptic origin has many problems in clinical practice. At the same time, an adequate assessment of the syndrome is extremely necessary to develop an optimal treatment strategy. In the focus of the most significant aspects of the problem of differential diagnosis of epileptic and non-epileptic paroxysmal sleep disorders, the main attention, from our point of view, should be concentrated on the following fundamentally important issues:
1. Epileptic and non-epileptic paroxysmal disorders are associated with disorders of the micro- and macroarchitecture of sleep (occur mainly in the slow-wave sleep phase - non-REM sleep, are associated with the phenomenon of “arousal” awakening, and are characterized by specific patterns in the form of K-complexes and vertex waves) .
2. Individual nocturnal paroxysms of epileptic and non-epileptic origin are similar both in clinical manifestations and in polysomnographic characteristics.
3. During nocturnal paroxysms of both epileptic and non-epileptic origin, the patient’s consciousness can be preserved or impaired.
4. Non-epileptic nocturnal paroxysms in some cases can bring more suffering to the patient than epileptic seizures.
It should be noted that nocturnal paroxysms of epileptic origin and many parasomnias have a close relationship with the phenomenon of awakening. Epileptic patterns that occur during the phase of rapid eye movement (REM sleep) and slow-wave sleep (non-REM sleep) are considered by a number of researchers as unique analogues of parasomnia (Clarenbach, Bukau, 1995). So-called “false” or pseudo-awakenings are characterized by the presence of K-complexes and vertex waves on the sleep EEG, which are regarded as epileptogenic (Niedermeyer, 1972). The role of sleep spindles is not well defined (Niedermeyer, 1995).
In recent years, in order to diagnose and differentially diagnose paroxysmal sleep disorders of epileptic and non-epileptic origin, as well as to analyze the semiology of attacks, the method of polysomnography with simultaneous video monitoring during sleep has been used (Niedermeyer, 1983; Broughton, 1987; Niedermeyer, Lopez da Silva, 1987). This method allows you to record both interictal and seizure EEG changes and the clinical condition of the patient. In clinical practice, the telemetry method (mobile long-term EEG), a combination of short-term recording of sleep EEG and mobile long-term EEG monitoring, is also used (Newzella, Platte, 1993).
In some cases, when it is difficult to differentiate between paroxysmal sleep disorder of epileptic and non-epileptic origin, it is recommended to prescribe the patient a “trial” anticonvulsant therapy, for example, carbamazepine. The patient's response (relief of attacks or absence of changes) allows the doctor to draw a conclusion about the nature of the existing paroxysmal disorder.
EPILEPTIC PAROXYSMS IN SLEEP
Gowers (1881) was the first to focus physicians' attention on the circadian distribution of epileptic paroxysms and identified attacks that occur during sleep, shortly after falling asleep, and upon awakening. Langdon-Down (1929) also emphasized the advisability of differentiating individual epileptic paroxysms, taking into account their relationship with the sleep-wake cycle. Janz (1962) proposed a classification of generalized epilepsies according to their relationship with sleep and awakening. Further differentiation of nocturnal paroxysms became possible thanks to the clarification of the semiology of attacks, the use of the polysomnography method, as well as a system of special application of electrodes (Luders et al, 1987). At the same time, a number of issues in the differential diagnosis of epileptic and non-epileptic nocturnal paroxysms remain insufficiently clarified.
There is a close relationship between epilepsy and sleep. 75% of all paroxysms occur during sleep (Clarenbach, Bulaun, 1995). Nocturnal epileptic paroxysms themselves often lead to various disturbances in the sleep profile. Changes in sleep characteristics are also observed under the influence of anticonvulsant therapy (Clarenbach et al, 1981; Wolf, 1987; Borbely, 1992). It has been shown that sleep can improve in some cases under the influence of anticonvulsant therapy (Johnson, 1982).
Epileptic brain activity contributes to both changes in sleep stages and the overall sleep profile (Baldy-Mouliner et al, 1984; Montplaisir et al, 1985; Dadmehr et al, 1987). In this case, clinical manifestations of paroxysms may be absent. The following sleep disturbances may occur due to nocturnal epileptic activity:
- increased and accelerated changes in sleep stages;
- fragmented R EM sleep;
- increased frequency of awakenings;
- decreased sleep efficiency (the relationship between sleep duration and night awakenings);
- shortening the total duration of sleep;
- prolongation of phases I and II of sleep;
- prolongation of sleep latency;
- disappearance of K-complexes and sleep spindles.
Epileptic seizures most often occur during the slow-wave sleep phase (non-REM sleep), particularly in stages I and II of sleep (Zeitihofer et al, 1991). Almost all primary generalized epileptic paroxysms, in comparison with complex partial seizures, are observed during slow-wave sleep (Montplaisir et al, 1985). The incidence of sleep disorders increases with the frequency of attacks. These disorders do not depend on the age of the patient (Horrner et al, 1984), but are often associated with the nature of the attacks. Patients with simple and complex partial paroxysms often have complaints of sleep disturbances.
Epilepsy and sleep have mutual influence on each other. In this regard, there are many problems in the diagnosis and differential diagnosis of nocturnal epileptic seizures:
- epileptic seizures that occur during sleep are often not regarded as epileptic or are not recognized at all;
- the semiology of epileptic paroxysms at night and during the day can differ significantly;
- individual nocturnal epileptic paroxysms are often mistakenly regarded as psychogenic;
- in some cases, during nocturnal epileptic seizures, the EEG does not show typical patterns.
Such diagnostic difficulties predetermine the need for special studies of nocturnal epileptic paroxysms based on sleep monitoring.
GENERALIZED EPILEPSY
Janz (1962) proposed a division of generalized paroxysms according to their relationship with the sleep-wake cycle into attacks that occur upon awakening, during sleep and diffuse ones, observed both during the day and at night. It should be noted that the circadian distribution of seizures may change as the disease progresses. Thus, attacks that occur upon awakening or during sleep may become diffuse; seizures observed on awakening evolve into seizures occurring during sleep. At the same time, “sleep epilepsy” almost never turns into “waking epilepsy” (Janz, 1962).
There are a number of epileptic syndromes in which seizures are associated with awakening: grand mal awakening (idiopathic generalized epilepsy with tonic-clonic seizures), absence seizures, juvenile myoclonic epilepsy, West syndrome (infantile spasms). In most cases (90%) “awakening epilepsies” are idiopathic genetically determined forms of epilepsy. Seizures usually occur 1-2 hours after waking up, after a daytime nap, or in the evening, between 6 and 8 p.m. (“end-of-working day epilepsy”) (Janz, 1962). It is characteristic that many patients who have attacks upon awakening wake up slowly in the morning, are often sleepy and become able to work after a certain interval of time. These patients prefer to go to bed late, fall asleep slowly, have difficulty reaching the superficial stages of sleep (stage III non-REM sleep), and only in the morning do they experience deep sleep.
Diffuse epilepsies, in which attacks do not have a clear circadian distribution, are symptomatic focal (temporal and frontal) epilepsies in 53% of cases.
Of particular interest are some forms of generalized epilepsies, in particular epilepsy with grand mal seizures during sleep and Lennox Gastaut syndrome, which were called “sleep epilepsies” by Janz (1962).
Clinical characteristics. Most grand mal attacks that occur during sleep are very mild and sometimes not recognized even during polysomnographic testing. In Lennox-Gastaut syndrome, nocturnal paroxysms are often characterized only by the opening of the eyes and tonic abduction of them upward, in some cases by tonic abduction of the head. The duration of such a paroxysm is no more than 10 seconds. Night attacks with Lennox Gastaut syndrome usually occur in the first half of the night, but then may become more frequent. Attacks of “sleep epilepsy” develop predominantly soon after falling asleep, between 22 and 24 hours, or 1–2 hours before awakening during non-REM sleep (Janz, 1974). Compared to patients suffering from epilepsy with awakening seizures, patients with “sleep epilepsy” wake up in the morning alert, fresh, and well rested. Their maximum performance is observed in the first half of the day. At the same time, they prefer to go to bed in the early evening and usually fall asleep early, quickly reaching the deep stage of sleep.
Data from laboratory and functional studies. A polysomnographic study reveals a reduction in sleep spindles and a shortening of the duration of REM sleep. During the non-REM sleep phase, fragmentary spike-wave complexes or generalized spike-wave complexes with a frequency of 3 Hz are recorded. Grand mal attacks most often occur during stage 1 non-REM sleep (Billiard, 1982). Typical EEG patterns are symmetrical synchronized sharp waves or temporal spikes. In Lennox-Gastaut syndrome, activation of epileptic activity is observed during sleep. Typical EEG changes are: focal or multifocal “sharp-slow wave” complexes with a frequency of 1-2.5 Hz with a strong tendency to generalize (Stefan, 1991).
Differential diagnosis. The most difficult is the differential diagnosis between nocturnal generalized attacks and nocturnal complex partial paroxysms. The “key” diagnostic signs for complex partial paroxysms—aura and disturbance of consciousness—cannot be adequately assessed at night. The presence of attacks, along with night and daytime, indirectly indicates the likelihood of complex partial paroxysms. The presence of focal changes in the sleep EEG testifies in favor of partial epileptic paroxysms. However, nocturnal partial paroxysms are often accompanied by rapid secondary generalization, making it difficult to identify focal EEG patterns. Particular difficulties arise in the differential diagnosis of generalized and frontal lobe epilepsies. Frontal paroxysms often occur with preserved consciousness. Typical for frontal epilepsy are: a high frequency of attacks, turning the head and eyes to the side, the presence of peculiar postures (the “fencer’s” pose) and automatisms (pedaling movements of the legs). To make a differential diagnosis between generalized and frontal lobe epilepsies, EEG video monitoring is necessary.
The differential diagnosis between primary generalized epilepsy and Rolandic epilepsy is based on the detection of typical “Rolandic” spikes localized in the centrotemporal region on the EEG. Differential diagnosis with electrical status epilepticus during slow-wave sleep (ESES) is not difficult, since ESES is characterized by specific typical EEG patterns - generalized spike-wave complexes, recorded in all leads throughout the curve (Patry et al, 1971) .
Treatment. In the treatment of epilepsy with grand mal attacks during sleep, the drug of first choice is sodium valproate. Phenobarbital is sometimes used. In the treatment of Lennox-Gastaut syndrome, sodium valproate, ethosuximide, and mesuximide are recommended. It is often necessary to resort to combination therapy with carbamazepine, phenytoin, primidone or phenobarbital. Additionally, ACTH and benzodiazepines are sometimes used (Matthes, Schneble, 1992).
FOCAL EPILEPSY
Temporal lobe epilepsy
Temporal lobe epilepsy is the most common form of focal epilepsy. Temporal lobe epilepsy can manifest itself as simple partial, complex partial and secondary generalized paroxysms. The following types of temporal lobe epilepsy are distinguished (Wieser, Hajek, 1995):
- hippocampal-amygdalar (mediobasal limbic);
- neocortical lateral temporal;
- opercular-insular.
Among the various types of temporal lobe epilepsy, the most common is mesial temporal lobe epilepsy (mediobasal limbic) (Wieser et al, 1993). It is important to note that hippocampal-amygdala temporal lobe epilepsies are activated by REM-CHOM (Wieser et al, 1993).
Clinical characteristics. Temporal paroxysms can be observed shortly after falling asleep (38% of cases), shortly after waking up (28%), or during the day (Janz, 1974). A typical sign of temporal lobe epilepsy is an aura. Most often, with temporal lobe epilepsy in children, an aura is noted in the form of a feeling of fear, unusual sensations (tickling) in the epigastric region, sensations of “already seen,” dream states, and less commonly, complex illusions and hallucinations (Wieser, 1987). Following the aura, a disturbance of consciousness often occurs. Oroalimentary automatisms (chewing, smacking, lip licking) are often observed, sometimes in combination with unilateral wrist automatisms and dystonic placement of the hand on the contralateral side (Kotagal et al, 1989). Autonomic symptoms such as increased heart rate and breathing are also characteristic. Secondary generalization is also possible.
Data from laboratory and functional studies. Typical EEG patterns in the interictal period are often absent. A polysomnographic study is necessary, which can detect epileptic activity (sharp waves or “sharp-slow wave” complexes) in 95% of cases (Gibbs, Gibbs, 1947; Sutherling, 1987). These EEG patterns appear most clearly in stages I-II of sleep and in the first sleep cycle (Passouant, 1967; Montplaisir, et al, 1980).
Differential diagnosis. The differential diagnosis of temporal lobe epilepsy and parasomnia (with somnambulism, nightmares, nocturnal enuresis, stereotypical head shaking, nocturnal paroxysmal dystonia) seems difficult. Compared with temporal lobe epilepsy, stereotypic head shaking and nightmares have an earlier age of onset. and paroxysmal nocturnal dystonia is later (Meier-Ewert, Schuiz, 1990). Nightmares often cause changes in heart rate and breathing rate.
Significant assistance in differential diagnosis is provided by laboratory research methods (NMR, positron emission tomography, photon positron emission tomography), which make it possible to detect structural damage to the temporal lobe (mesial temporal sclerosis) (Cascino et al, 1991). In some cases, for the differential diagnosis of temporal lobe epilepsy and parasomnias, a trial prescription of anticonvulsants is also recommended (Roder, Wolf, 1981). The lack of effect when prescribing anticonvulsants is more evidence in favor of narasomnia. One of the main differential diagnostic methods is EEG recording during sleep, which makes it possible to identify patterns typical for temporal lobe epilepsy that are absent in parasomnias. It should be noted, however, that with superficial application of electrodes it is not always possible to detect temporal lesions. In this regard, in some cases, the use of sphenoidal, subdural and intracerebral electrodes is recommended.
Treatment. The first-line drugs of choice for the treatment of temporal lobe epilepsy are carbamazepine and phenyin (Matthes, Schneble, 1992). For temporal epileisias that are resistant to anticonvulsant therapy, neurosurgical correction is recommended (Engel, 1987).
Frontal epilepsy
Clinical characteristics. Frontal paroxysms are characterized by a number of features that distinguish them from paroxysms of other localization: sudden (often without an aura) onset, high frequency of attacks with a tendency to be serial, short duration (30-60 sec), often preserved consciousness, vocalization, elaborate motor automatisms and postures , pronounced stereotypicality of attacks, absence or minimal post-attack confusion. Frontal seizures often occur during sleep (Baldy-Mouliner, 1986). Consciousness at the time of paroxysm is often preserved, and some patients are able to describe or even depict their attacks (Shondienst, 1995). Many patients are quite indifferent to attacks.
A special place among frontal paroxysms is occupied by attacks emanating from the supplementary motor area. The supplementary motor area is located between the paracentral lobules and the cingulate gyrus (PenField, Welch, 1951). It presents a somatotopic projection of various parts of the body. Seizures emanating from the supplementary motor area, like other frontal paroxysms, occur predominantly at night. Tonic motor phenomena dominate in the proximal parts of the upper and lower extremities, pretentious postures and automatisms in the form of flapping hands, wheel-like rotation of the whole body (Lim et al, 1991). A typical “fencing pose” is often noted. Intelligence is usually not affected (Chauvel et al, 1992).
Data from laboratory and functional studies. In EEG studies, pathological epileptic patterns are often absent (Mayer, Schondienst, 1993). A significant number of artifacts are often recorded on the seizure EEG, which complicates the interpretation of the data (Morris et al, 1988). EEG using special electrodes (subdural, intracerebral) is more informative.
Differential diagnosis is carried out with various syndromes of both epileptic and non-epileptic origin (generalized epilepsy, temporal lobe epilepsy, pseudoepileptic seizures, nightmares).
Pseudoepileptic seizures, in comparison with frontal paroxysms, rarely occur at night, have a longer duration and are not stereotypical (Kanner et al, 1990).
Nightmares occur between the ages of 4 and 12 years, usually occurring in the first third of the night and never during the daytime. Attacks of nightmares are characterized by the absence of an aura, motor automatisms, and partial impairment of consciousness. At the time of the attack, vegetative symptoms are expressed - tachycardia, tachypnea. The duration of nightmare attacks is 5-6 minutes. An EEG study during nightmares does not reveal epileptic patterns.
Differential diagnosis between frontal and temporal paroxysms is based on the following criteria: the presence of an aura, the nature of automatisms, impaired consciousness, duration of attacks, the presence of post-attack confusion. With temporal attacks, in comparison with frontal ones, auras, oroalimentary automatisms are often observed, consciousness is often impaired, post-attack confusion, and a longer (1-4 minutes) duration of paroxysm.
When differential diagnosis with primary generalized epilepsies, the semiology of seizures should be taken into account. The EEG is not always sufficiently informative, since frontal paroxysms tend to undergo rapid secondary generalization (Holthausen, 1995).
Treatment. The first-line drugs of choice for the treatment of frontal lobe epilepsy, as well as temporal lobe epilepsy, are carbamazepine and phenytoin.
ESES (electrical status epilepticus during slow sleep) Electrical status epilepticus during slow sleep
Patry et al in 1971 described peculiar EEG patterns in the form of “electrical status epilepticus” (ESES). Later, Tassinari et al (1977, 1982), Billiard et al (1982) presented a clinical description of the syndrome, calling it “epilepsy with prolonged spike-wave complexes during slow sleep” (CSWS-continuos spike-wave during slow sleep). Under this name, the disease was included in the International Classification of Epilepsies and Epileptic Syndromes. In recent years, it has been established that ESES is an electrographic diagnosis and in some cases may not be accompanied by clinical manifestations.
Clinical characteristics. The disease manifests itself at the age of 8 months to 11.5 years (Tassinari et al, 1985), more often between 4 and 14 years (Morikawa et al, 1985, 1989). After 15 years, the syndrome usually does not occur (Tassinari et al, 1985; Morikawa et al, 1989). Often attacks occur at night. By nature, attacks can be either generalized or partial. Depending on the semiology of attacks, Tassinari et al (1994) identified 3 groups of patients:
1. Patients with only motor seizures (myoclonic absences, generalized clonic seizures, orofacial paroxysms). 2. Patients with initially unilateral partial motor seizures or generalized tonic-clonic paroxysms in combination with atypical absences, which develop as the disease progresses. 3. Patients with nocturnal generalized tonic-clonic seizures in combination with atypical absences and atonic paroxysms. The frequency of attacks is variable - from rare to daily.
Data from laboratory and functional studies. On interictal EEG in a state of wakefulness, generalized spike-wave complexes are recorded, sometimes in the form of flashes, or focal spikes or sharp waves with a predominant localization in the frontotemporal or centrotemporal regions (Tassinari et al, 1994). During slow-wave sleep, the EEG shows prolonged (85-100% of the entire curve), bilateral or diffuse “spike-wave” complexes. Physiological sleep patterns (sleep spindles, K-complexes or vertex waves) are practically absent (Tassinari et al. 1994).
Differential diagnosis should be made with Landau-Kleffner, Lennox-Gastaut syndromes, and Rolandic epilepsy. The most difficult is differential diagnosis with Landau-Kleffner syndrome. With Landau-Kleffner syndrome, speech disorders and behavioral disorders come to the fore. The nature of the attacks is usually atonic, while with ESES syndrome, generalized tonic-clonic, atypical absences are most often observed. The question of the possible transformation of ESES syndrome into Landau-Kleffner syndrome is being discussed (Shoumaker et al, 1974; Kellerman, 1978; Hirsch et al, 1990).
In some cases, with ESES syndrome, both daytime and nighttime seizures are observed, combined with speech disorders, which predetermines the need for differential diagnosis with Rolandic epilepsy. The most significant differential diagnostic criteria are the absence of neuropsychological disorders in rolandic epilepsy and the presence of specific spike patterns on the EEG with a predominant localization in the centrotemporal regions. In ESES syndrome, focal EEG changes are recorded predominantly in the frontal areas (Tassinari et al, 1985).
In ESES syndrome, in comparison with Lennox-Gastaut syndrome, there are no tonic seizures and slow spike-wave complexes with a frequency of 2-2.5 Hz (Patry et al, 1971).
Treatment. The order of choice of drugs depends on the nature of the attacks. In the presence of atypical absence seizures, sodium valproate and ethosuximide are recommended; for partial paroxysms, carbamazepine or phenytoin is recommended.
Continued >>
Different forms of seizures
When considering the syndrome of paroxysmal states, it is worth paying attention to those diseases that most often accompany such crises.
- headache;
– myoclonic syndromes and other hyperkinetic states;
– autonomic disorders;
– muscular dystonic syndromes and dystonia.
In most cases, these problems are recorded in patients who have not reached the age of majority. But recently, more and more often, the paroxysmal state makes itself felt for the first time already in adulthood. It is also possible for the symptoms of the above diseases to dynamically progress, which become more severe against the background of chronic and acute cerebrovascular accidents or age-related cerebral disorders.
It is also important to take into account the fact that in some cases, non-epileptic paroxysmal conditions may be a consequence of the effects of certain medications prescribed to neutralize circulatory failure, as well as diseases such as parkinsonism and some mental disorders caused by old age.
Epilepsy is not the only form of manifestation of disorders of the central nervous system. There are other paroxysmal conditions in neurology that can be classified as epileptic.
One striking example is sensory (sensitive) Jacksonian seizures. Their manifestation occurs when a person is conscious. Symptoms include tingling and numbness in the face, limbs and half of the torso. In some cases, sensory seizures can turn into motor ones, which will significantly complicate the patient’s condition.
Attention should also be paid to Jacksonian epilepsy. In this case, both sensory and motor seizures are possible. The latter are especially problematic because they involve muscle spasms in the part of the face and limbs that are located on the side opposite the epileptic focus. In this case, disturbances in consciousness, as a rule, are not observed. In some cases, motor seizures can become generalized.
Complex absence seizures can be atonic, myoclonic, or akinetic. The first make themselves known through a sudden fall, the cause of which is a sharp decrease in the postural tone of the legs. As for the myoclonic form, it is characterized by rhythmic short-term muscle twitching, accompanied by a loss of consciousness. Akinetic absence seizure is a seizure with immobility, which can also result in falls.
Small absence seizures are also possible, in which a person also plunges into an unconscious state. There are no feelings of discomfort after its completion. The patient often cannot remember the moment of the attack.
Kozhevnikov epilepsy is characterized by limited short seizures that are clonic in nature. They most often capture the muscles of the arms, but the tongue, face and even legs can be affected by this process. Loss of consciousness during such convulsions is a rare occurrence.
Such paroxysmal activity can be divided into several types - muscle dystonia, autonomic disorders, headaches, myoclonic syndromes. They usually first appear at a young age and progress in old age.
This is usually affected by cerebrovascular accidents seen in older people. Therefore, to prevent such conditions, patients are prescribed drugs in advance to activate cerebral blood flow. This is done with extreme caution, since the wrong medicine can provoke a seizure.
- headache;
– myoclonic syndromes and other hyperkinetic states;
– autonomic disorders;
– muscular dystonic syndromes and dystonia.
Epilepsy is not the only form of manifestation of disorders of the central nervous system. There are other paroxysmal conditions in neurology that can be classified as epileptic.
Kozhevnikov epilepsy is characterized by limited short seizures that are clonic in nature. They most often capture the muscles of the arms, but the tongue, face and even legs can be affected by this process. Loss of consciousness during such convulsions is a rare occurrence.
Treatment of paroxysmal conditions is the domain of highly qualified specialists. Therefore, if signs of a single seizure become noticeable, especially when it is the first, the patient must be urgently hospitalized in a neurosurgical or neurological department. There they will be able to examine him and determine the current treatment plan.
It is important to ensure that the patient does not suffer any injuries before being taken to the hospital. It is also worth putting a spoon wrapped in a bandage into the mouth or using a mouth dilator.
In most cases, the treatment process for patients with status epilepticus begins in the ambulance. If doctors are not yet around, and the person is still having a seizure, then the first thing to do is to rule out the possibility of aspiration of vomit or mechanical asphyxia due to tongue prolapse.
As for non-epileptic forms, the causes of paroxysmal states can be completely different. It all depends on the key disease, the symptoms of which are aggravated. Therefore, the best thing that can be done is to take the person to the hospital as quickly as possible, where he can be examined and an accurate diagnosis made.
Paroxysmal states in neurology and psychiatry
Summary
From April 18 to April 25, 2005, the Russian National Congress “Man and Medicine” was held in Moscow, within the framework of which the pharmaceutical industry (Croatia) held an interdisciplinary symposium dedicated to the role of modern anticonvulsants in neurological and psychiatric practice.
The reports at the symposium covered the clinical picture of a number of paroxysmal and painful conditions, as well as the features of their treatment. Currently, drugs are widely used in the treatment of nervous and mental disorders due to their antiepileptic, normothymic, antidepressant and analgesic effects, but their use should be based on accurate topical diagnosis, correct dose selection, and consideration of the patient’s general somatic condition. We present to our readers a brief overview of the symposium reports.
Doctor of Medical Sciences, Professor of the National Scientific Center for Narcology of the Russian Federation Vladimir Borisovich Altshuller reported on the peculiarities of the use of anticonvulsants in drug treatment practice.
- There are two main ways to use anticonvulsants in a drug treatment clinic. The first way is traditional and consists of using these drugs to treat alcohol withdrawal syndrome. The second is the use of anticonvulsants to suppress pathological craving for alcohol (PCA), primarily primary, which is considered one of the main tasks of narcology, since it is this form of PCA that is of great importance in the formation of alcoholism.
Dysphoric conditions play a significant role in the pathogenesis of PVA. The similarity of these conditions with epileptiform conditions determines the choice of therapeutic agents with antiepileptic properties. In addition to PVA, the point of application of anticonvulsants in drug treatment practice is alcoholism with epileptic seizures.
Despite the fact that the pathogenesis of alcoholic epilepsy has received sufficient attention, some aspects of it still remain unclear. In particular, the question of the etiology of the disease has not been resolved. American authors explain alcoholic epilepsy with the neuronal kindling hypothesis. Its essence lies in the fact that during repeated withdrawal states, stimulation of limbic structures is systematically repeated, as a result of which the reaction of these formations intensifies, the symptoms become more severe and complicated, epileptiform activity arises and gradually stabilizes with a focus in the hippocampus and tonsils, spreading to other parts of the brain and persisting beyond abstinence.
In the 80s, the NSC Narcology described a paroxysmal variant of the dynamics of PVA. It is known that PVA exists in various variants, which include obsessive, hallucinatory and paranoid states, and often their dynamics are similar to manic-depressive psychosis. The paroxysmal variant often occurs in women in the later stages of severe alcoholism. Its distinctive feature is the occurrence of paroxysmal and relatively short-term, very intense craving for alcohol. The abundance of vegetative reactions (pallor of the skin, dizziness, palpitations, etc.), affective saturation, some narrowing of consciousness, and sometimes partial amnesia give these states a great resemblance to epileptiform paroxysms of a diencephalic nature.
Patients with such disorders have a fairly complicated medical history: parental alcoholism, early age of onset of alcohol intake, high progression, lack of remissions, frequent relapses, decreased social functions.
In addition to manifest paroxysms, PVA is often observed in the clinic of female alcoholism in a form where the tendency to form periodic (binge) forms of drunkenness, the rudiments of paroxysms, which are manifested by the impulsiveness of desire - the suddenness and unaccountability of the initial intake of alcohol, are more pronounced. If manifest paroxysms of desire are rare and occur only in the later stages of alcoholism, then impulsivity is a more common phenomenon. Taking into account the experimental data on the epileptiform nature of the nervous process underlying PVA, we can assume the existence of a certain continuum of paroxysmalness - from rare manifest attacks of craving for alcohol to their more common rudimentary manifestations and further to a subclinical paroxysmal process that determines the banal pathological craving for alcohol.
The syndrome of emotional psychological disorders (alcoholic depression, drunken depressive-dysphoric states), which is widely represented in the alcoholism clinic, is of particular importance. Therefore, when using anticonvulsants, preference should be given to drugs with normothimic properties. These drugs of choice include carbamazepine, valproic acid, and lamotrigine.
Finlepsin (carbamazepine) differs from other anticonvulsants in its wide therapeutic range. It is used not only for the treatment of convulsive and psychomotor (so-called temporal lobe) forms of epilepsy, but also for trigeminal neuralgia, dysphoric conditions, acute schizophrenic psychoses with polymorphic affective symptoms, alcoholic delirium and alcohol withdrawal syndrome, as well as for the treatment of depression and mania. The latter is associated with its effect on the emotiogenic zones of the brain - limbic structures, which is especially important since it is here that the focus of epileptiform activity is localized, which is presumably the basis of PVA in patients with alcoholism.
When using Finlepsin, the vegetative stigmas of PVA are quickly reduced: sleep disturbances, alcoholic dreams, facial reactions, vasomotor and secretory reactions disappear. To a certain extent, it is also possible to stop psychopathic-like disorders within the framework of a painful attraction to alcohol (conflict, desire for early discharge, evasion of treatment, etc.). Mild forms of behavioral disorders are eliminated first, and only then moderate and severe ones. An explanation for this can be a well-known clinical pattern: pathological attraction to psychoactive substances is formed and realized through the patient’s personality, especially with regard to behavioral aspects. The so-called alcoholic thinking, if it is a component of a pathological craving for alcohol, is significantly corrected under the influence of Finlepsin.
Convulsofin is one of the most effective treatments for epilepsy, including its convulsive and non-convulsive forms. The drug’s ability to eliminate anxiety, dysphoria, and tremor is known. There is information about the therapeutic use of Convulsofin in bipolar affective pathology, in manic and depressive states. In other words, Convulsofin, like Finlepsin, has not only anticonvulsant, but also psychotropic, or more precisely, emotiotropic effects.
The Research Center for Narcology used a technique developed at the Institute of Higher Nervous Activity of the Russian Academy of Medical Sciences, which is based on computer analysis of the EEG, sampling the required rhythm. The delta rhythm was assessed, since its wave characteristics are most indicative of paroxysmal activity. There is evidence of high intensity of the delta rhythm in patients with alcoholism. It has been verified that during exacerbation of PVA, the delta rhythm increases, and after the use of an anticonvulsant, its intensity decreases.
As a result of the use of Finlepsin and Convulsofin, it turned out that these medications in relatively small doses that do not cause side effects have a rapid, often reversing effect, suppressing PVA. High effectiveness was shown in cases where the craving for alcohol was clearly periodic in nature, with a rich affective coloring or signs of paroxysmalness.
Thus, some of the anticonvulsants can be effectively used in the treatment of patients with alcoholism. The anticonvulsants proposed to relieve exacerbations of PVA are distinguished by a sharp predominance of anticonvulsant activity over the general inhibitory effect (the latter is either extremely insignificant or practically absent) and have a therapeutic effect precisely due to this property, since high mental tone is a necessary prerequisite for the successful suppression of the desire for alcohol.
The problem of treating pain syndromes in neurology was discussed in a report by Vladimir Alekseevich Karlov, corresponding member of the Russian Academy of Medical Sciences, Doctor of Medical Sciences, Professor of the Moscow State Medical Dental University.
- The use of carbamazepine in the USSR began in 1969 after the appearance of the original drug Tegretol on the market. It was subsequently replaced by Finlepsin, which today remains the main drug from the carbamazepine group in the treatment of trigeminal neuralgia and epilepsy. Carbamazepine has shown its clinical effectiveness in the treatment of symptomatic and cryptogenic forms of epilepsy with focal, primary and secondary generalized types of seizures. Carbamazepine is currently widely used to treat trigeminal neuralgia, occipital neuralgia, postherpetic neuralgia, and diabetic polyneuropathy. It is also prescribed for affective disorders, such as manic psychosis and bipolar states, which is explained by the normothimic properties of carbamazepine. The structure of the drug molecule, which is similar to diazepam, determines its psychotropic effect.
Carbamazepine, which is not an analgesic, has a pharmacospecific antiparoxysmal antianalgesic effect in paroxysmal neuralgia.
For trigeminal neuralgia, carbamazepine was first used by Blom in 1962. MGMSU conducted its own studies of the effects of carbamazepine (O.N. Savitskaya, V.A. Karlov, 1970-1975). Long-term use of carbamazepine in 93 patients with trigeminal neuralgia, including those with a disease duration of more than five years, showed that complete cessation of pain for one period or another was noted in 40% of patients, marked improvement in 55%, and no effect. at 5%.
In our other observations on 28 patients, studying the effect of Finlepsin in trigeminal neuralgia, the results on the 6th month of treatment were as follows: good effect - in 43% of patients, satisfactory - in 36%, no effect - in 14%, side effects - in 18% of people. In 7% of cases the drug had to be discontinued due to intolerance.
In recent years, sufficient data have been accumulated on the use of carbamazepines in neurological practice, in particular for postherpetic neuralgia (additive therapy). The most effective drug for diseases accompanied by the presence of painful paroxysms (50% of cases) and in patients with allodynia was the drug Finlepsin. The effect on painful paroxysms with allodynia was achieved in two thirds of patients.
Carbamazepine was tested in acute bipolar disorders (Okuma, 1970; Krober, 1983; Neppel, 1987; Post, Weiss, 1987), and its effect was compared with lithium (Okuma, 1988; Small et al., 1991) and haloperidol (Goncalves, Stole , 1985; Brown, 1987). According to these studies, the effectiveness of carbamazepine is not inferior to that of traditional drugs, but it was better tolerated by patients.
Preliminary results of a study of the comparative effectiveness of domestic carbamazepines and Finlepsin, conducted at MSMSU, showed a higher effectiveness of the latter. Thus, carbamazepine is the first choice drug for symptomatic epilepsy with partial and secondary generalized seizures, and paroxysmal cranial neuralgia. It is also a competing drug for mood disorders.
Doctor of Medical Sciences, Head of the Department of Neurology of the Pediatric Faculty of the Russian State Medical University, Professor Andrei Sergeevich Petrukhin devoted his report to modern treatment of partial types of epilepsy.
- Focal forms of epilepsy include epilepsy with central temporal spikes and epilepsy with occipital paroxysms. Recently, symptomatic variants have been identified, epilepsy with severe migraine and cryptogenic forms of unknown etiology. Symptoms depend on localization and manifest as simple and complex partial and secondarily generalized convulsive seizures. There are symptomatic frontal, parietal, temporal, and occipital epilepsies. Making a topical diagnosis is complicated by the migration of epileptiform activity due to the interaction of different parts of the brain.
Idiopathic forms, such as rolandic epilepsy and Gastaut syndrome, are relatively benign and respond well to treatment (up to 95-95% complete remission). The basic drug for rolandic epilepsy is valproic acid, and for Gastaut syndrome - carbamazepine.
Frontal symptomatic epilepsy is the most difficult to diagnose. Its clinical picture consists of a sudden onset, the patient assumes abnormal postures, hypermotor attacks are observed, and speech disorders are possible. Lateral neocortical temporal lobe epilepsy occurs with auditory hallucinations and temporal syncope (loss of consciousness). Parietal epilepsy is characterized by sensory seizures that spread to neighboring lobes of the brain, which makes diagnosing this form difficult.
Symptomatic occipital epilepsy most often occurs due to brain tumors and herpes infection. With this form, attacks of eye deviation and migraine-like headaches develop.
The choice of drug depends on the form and topic of the disease, the type of attacks. The frequency of taking the drug is determined by the release form; preference should be given to retard forms.
The importance of correct topical diagnosis is emphasized by the varying effectiveness of antiepileptic drugs depending on the form of epilepsy. Carbamazepines are most effective for occipital epilepsy. Parietal and frontal forms of epilepsy respond better to treatment with Finlepsin. The dosage of the drug is 15-20 mg/kg body weight. The advantages inherent in Finlepsin retard are that the process of absorption of the retard form begins almost immediately, unlike other forms, constant concentration throughout the day avoids dose-dependent side effects, and also allows the patient not to be tied to the time of taking the medicine.
Treatment of symptomatic epilepsy lasts at least three years. Before discontinuing the drug, it is necessary to monitor the state of the patient’s nervous system and the presence of possible side effects. Since the range of manifestations of the latter is quite wide, international recommendations limit the combined treatment of epilepsy to the simultaneous use of no more than three antiepileptic drugs.
Candidate of Medical Sciences Zoya Vyacheslavovna Chernyak (Clinic of Nervous Diseases named after A.Ya. Kozhevnikov, Moscow Medical Academy named after I.M. Sechenov, head - Academician of the Russian Academy of Medical Sciences N.N. Yakhno) raised the issue of the effectiveness and safety of using Konvulsofin (calcium valproate) in neurological practice.
- Epilepsy is one of the most common diseases of the nervous system with a variety of clinical manifestations, different courses and prognosis. Epidemiological studies indicate a high incidence rate in all age groups. The prevalence of the disease in the adult population is 40-70 cases per 100 thousand population. The relevance of correct selection of therapy is emphasized by the possibility of achieving remission in 70-80% of cases. The main anticonvulsants are carbamazepines and valproates.
Valproic acid derivatives have been used to treat epilepsy for more than 20 years. Their undoubted advantage is their wide therapeutic effect. Traditionally, valproates are the first choice drugs for the treatment of generalized epilepsies, but they have also shown their effectiveness in the treatment of focal epilepsy. Unlike carbamazepine, valproates do not cause myoclonic seizures; they can be used for the purpose of muscle relaxation. Based on this, it is proposed to use valproate as the first choice drugs for the treatment of all forms of epilepsy. The mechanism of action of valproates is associated with a disruption of GABA metabolism by blocking GABA transferase, which leads to an increase in the content of GABA in the central nervous system and inhibition of the mechanisms of propagation of excitation in epileptogenic foci of the cerebral cortex.
Recently, the high effectiveness of a valproic acid derivative, the drug Convulsofin, produced by the German company AWD, has been noted. pharma. 1 tablet contains 300 mg of calcium salt of valproic acid. Fast and good absorption of the drug allows you to achieve a therapeutic plasma concentration of 50-100 mcg/ml 2-3 hours after taking the drug.
To assess the safety of using Convulsofin in neurological practice, we examined 97 patients with epilepsy in 2002-2003. The majority of patients were adults (73), their average age was 32 years, children (24 people) were 11 years old. Among the subjects, women predominated (61%). The patients were divided into two groups: patients with generalized - 38 people (39.2%) and patients with focal epilepsy - 59 (61%).
According to the form of generalized epilepsy, the patients were distributed as follows: the majority were patients with isolated generalized convulsive seizures, 10 people with childhood absence epilepsy, 9 with juvenile absence epilepsy and 5 with juvenile myoclonic epilepsy. Among the focal forms, temporal lobe epilepsy predominated.
39 patients were prescribed Convulsofin as initial therapy, since they had not previously received any other drug treatment; 36 patients received Convulsofin as a replacement for other ineffective or poorly tolerated drugs and 22 patients - as an additional therapy. Initial therapy was carried out at a dose of 5-10 mg/kg/day, achieving an average therapeutic dose of 750-2100 mg/day, which corresponded to 15-20 mg/kg/day in adults and 25-30 mg/kg/day in children. .
The effectiveness of Convulsofin was assessed according to the following criteria: complete absence of attacks, a reduction in their frequency by more than 50%, a reduction in frequency by less than 50% and no effect.
The total effectiveness in epilepsy reached 75%, in the group of generalized epilepsy - over 80%. In the generalized epilepsy group, 31 people were completely free of seizures, 6 had a decrease in their frequency by more than 50%, and 1 had a decrease in their frequency by less than 50%. In general, our results are consistent with data from similar studies showing that Convulsofin is quite effective in the generalized form of the disease, especially in childhood absence epilepsy.
The total effectiveness in focal epilepsy reached 60%. The following results were obtained: in 10 people there was an absence of seizures, in 26 - a decrease in their frequency by more than 50%, in 18 - by less than 50% and in 6 people (with frontotemporal epilepsy) there was no effect.
When replacing phenobarbital with Convulsofin, the frequency of seizures decreased in 70% of patients and tolerability improved in 10% of patients. When switching from carbamazepine, 78% of patients noted better tolerability.
According to EEG data (routine EEG, EEG after sleep deprivation and EEG video monitoring), epileptiform activity was detected in the majority of patients with generalized (87%) and focal (67%) epilepsy. 3 months after treatment with Convulsofin, epileptiform activity was detected in only 6% of individuals (in patients with focal epilepsy).
During our study, minor side effects were observed when using Convulsofin: weight gain, alopecia, dyspeptic disorders and menstrual irregularities, which, however, did not require drug replacement. We monitored clinical blood tests, biochemical parameters (AST, ALT, creatinine, total bilirubin), coagulogram before the start of treatment and 3, 6, 9 months after the start of therapy. Thrombocytopenia (12 cases), hypofibrinogenemia (14 patients), increased ALT, AST (12 patients) were noted.
Thus, Convulsofin is effective in almost all forms of epilepsy; when other valproates are replaced with Convulsofin, seizures decrease. This fact was confirmed in the works of foreign authors (Helene Klepel, H. Gebelt, D. Hobush, 1983; G.G. Shanko, S.E. Zyl, 2001). The use of Convulsofin is beneficial from the point of view of pharmacoeconomics; since January 2005 it has been included in the Federal Program for Social Security of the Population.
Epilepsy and paroxysmal conditions
This is a rather difficult diagnosis in terms of the level of its negative impact on a person. But first, it’s worth remembering what epilepsy is. We are talking about a chronic pathological disease of the brain, which is characterized by seizures that have a different clinical structure and are constantly recurring. This condition is also characterized by psychopathic paroxysmal and non-convulsive manifestations.
It is possible to develop two forms of epilepsy: genuine and symptomatic. The latter is a consequence of traumatic brain injury, intoxication, brain tumors, acute circulatory disorders in the head, etc.
It is worth understanding that the special relationship between the epileptic focus and different parts of the nervous system determines the occurrence of repeated seizures of various clinical structures. Some features of the pathological process can lead to this result.
In addition, other paroxysmal conditions may occur
How to treat paroxysmal supraventricular tachycardia
There are several treatment options at the FMBA center. Depending on the severity of the illness, the attending physician may place you in the therapeutic department. You will be under the constant supervision of professionals and receive timely medical care. This is usually drug therapy. If the symptoms of standard therapy are not enough, then you may be offered catheter ablation of the arrhythmia. At the same time, by puncture access under local anesthesia, under X-ray control using a catheter, an accurate diagnosis of the source of arrhythmia is made and, by precisely influencing it with a radiofrequency pulse or cold, the cause of paroxysmal tachycardia is eliminated.