How does a brain abscess develop?
There are several options for the development of a brain abscess:
- hematogenous (inflammatory processes in the lungs, gastrointestinal infections and sepsis);
- through infection as a result of traumatic brain injury;
- purulent-inflammatory (caused by inflammation in the nose and ears);
- infected (complications after neurosurgical interventions).
After infection penetrates, an abscess forms within three weeks and has the following stages:
- The first three days: the development of encephalitis (local tissue inflammation), which can be eliminated with antibacterial therapy.
- Days 4-9: inflammation progresses, the cavity filled with pus increases.
- 10-13 days: the formation of a protective capsule around the purulent focus, this prevents the process from spreading.
- Third week: compaction of the capsule with pus. Depending on the treatment taken at this stage, the brain abscess may begin to develop in the opposite direction or increase in size, and new foci of inflammation may also begin to appear.
Symptoms of a brain abscess
The difficulty of independently detecting a brain abscess is that it does not have unique symptoms, but only those that can be attributed to any other inflammatory diseases or brain diseases:
- general malaise;
- weakness;
- chills;
- vomit;
- apathy;
- headache;
- eye irritation from light;
- increased intracranial pressure;
- mental disorders, nervousness.
Therefore, if the above symptoms appear, you should consult a doctor as soon as possible. When a specialist diagnoses an abscess, the main reason for a more accurate examination will be the presence of an inflammatory process, which is accompanied by the appearance of neuropsychiatric disorders. To diagnose a brain abscess, the following are used:
- CT scan;
- MRI of the brain;
- MS spectroscopy;
- Ophthalmoscopy (detection of signs of intracranial pressure);
- Blood test (detecting signs of inflammation).
As a result of the diagnosis, the stage of the brain abscess will be determined and treatment will be selected.
Magnetic resonance imaging (MRI) in St. Petersburg
MRI of the brain. T2-weighted axial MRI. Multiple sclerosis. Color processing of the image.
Radiation diagnostics does not allow us to speak with a high degree of certainty about the pathogen; for this, bacteriological methods and detection of antibodies are used. At the same time, radiation diagnostic methods make it possible to talk about the extent of the lesion, complications and monitor the effectiveness of treatment. From the point of view of morphological changes, the infectious origin causes changes mainly such as meningitis, encephalitis, and brain abscess. MRI of St. Petersburg allows you to choose the location of tomography, and we have very extensive experience in MRI examination of the brain for infections. and MRI of the brain are the most important methods for morphological assessment of the state of the brain. Ultrasound duplex scanning is an additional method used when it is necessary to assess blood flow. The latter suffers mainly from cerebral edema. In addition, the infection may be complicated by arterial or venous thrombosis.
Bacterial infections
Meningitis
Meningitis is an inflammation of the lining of the brain. Usually accompanied by inflammation of the lining of the ventricles - ventriculitis. Inflammation of the arachnoid membrane leads to disruption of the blood-brain barrier, isolation from the body’s immune system, and increased vascular permeability. As a result, swelling and impaired blood supply develop. Pathogens: in newborns - streptococci (over 60%) and E. coli, in children - hemophilus and Nysseria (meningococcus), in adults - streptococcus pneumonia and Nysseria. In addition to bacterial ones, there are viral, tuberculous and fungal meningitis. Routes of penetration of the pathogen: hematogenous (usually the nasopharynx), extracerebral - through the inner ear (otitis media, mastoiditis, sinusitis) and direct - infection during surgery. The frequency is 0.25-1 per 1000 in newborns, 4-6.5 per 100 thousand in children, about 4 per 100 thousand in adults. 70% up to 5 years. Mortality varies greatly depending on the pathogen, the severity of infection, the age of the patient and the state of immunity. If the effectiveness of antibacterial therapy is insufficient, it reaches 15-30%.
Clinical manifestations consist of headaches, fever, and may include nausea, vomiting (35%), convulsions (30%), and impaired consciousness. Very sharp start. In the neurological status, meningeal signs are determined (50%). The main diagnostic method is lumbar puncture and CSF examination. CT and MRI have a role in identifying complications. Complications are observed in 50% of patients - these are venous sinus thrombosis, arterial or venous infarction (30%), cerebritis and brain abscess, subdural accumulation of exudate (20-50%) and empyema (2%), ventriculitis (newborns - 92%, adults – 30%), hydrocephalus, cerebral edema. Non-contrast CT and MRI for uncomplicated meningitis are insensitive in 50% of cases, in other cases they reveal hydrocephalus, swelling of the gyri, widening of the interhemispheric fissure, and obliteration of the cisterns. After contrasting, there is an enhancement of the membranes (pachymeningitis) and, sometimes, the grooves (leptomeningitis). With duplex scanning, an increase in resistance indices indicates increased intracranial pressure.
Brain abscess
ICD-10 considers brain abscess as an independent disease. However, the first stage of brain damage caused by a purulent infection is cerebritis. Its early stage lasts 3-5 days and is not accompanied by macroscopic changes. In the late stage of cerebritis (days 5-14), an area of necrosis forms. After the 14th day, an abscess capsule gradually forms. The mortality rate from brain abscess is 5-50%, depending on the effectiveness of antibiotic therapy.
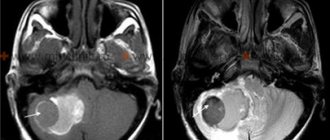
CT and MRI in the early stages of cerebritis reveal edema, there may be parenchymal contrast, in the late stage - central necrosis and peripheral edema, peripheral contrast is noted. The formed abscess has a contrasting capsule, its walls are smooth, their thickness is up to 5 mm. On DWI-type MRI, the contents of the abscess are bright, which distinguishes them from intratumoral necrosis.
| MRI of the brain. Brain abscess. Axial MRI type FLAIR. | MRI of the brain. Axial T1-weighted MRI with contrast. Brain abscess. | MRI of the brain. Brain abscess. Axial diffusion-weighted MRI. |
Venous sinus thrombosis
Venous sinus thrombosis is a consequence of occlusion of the sinus and/or cortical vein. Pathogenesis is associated with external compression (edema during infection, tumor invasion) and partial thrombosis (hypercoagulation). The consequence of venous thrombosis is a heart attack with a hemorrhagic component. The typical localization of infarctions in superficial vein thrombosis is at the junction of the white and gray matter, and in deep vein thrombosis (Rosenthal) - symmetrically in the visual thalamus. The mortality rate is very high.
On non-contrast CT scans, a thrombus is sometimes visible in the form of a “delta sign” - a dense triangular area (usually in the superior sagittal sinus). Contrast-enhanced CT scans show a “reverse delta sign,” that is, an unenhanced triangle. Only both signs together have diagnostic value. Additionally, venous infarctions may be detected.
CT. Hypodense area of infarction in the left temporal lobe. Hyperdense triangular area in the left transverse sinus.
On non-contrast MRI of the brain, a thrombus is visible in the form of an area of hemorrhage, the signal from which depends on the period. MR venography demonstrates absence of blood flow. With MRI, false-positive results are common due to congenital sinus hypoplasia, leak-in effect (loss of signal) and developed arachnoid granulations.
| MRI of the brain. Hyperintense with hemorrhage (dark deoxyhemoglobin) infarct area in the left temporal lobe on T2-dependent MRI images. | Lack of blood flow in the left transverse sinus with MRI. |
Arachnoiditis
Arachnoiditis is a general term that reflects inflammation of the membranes. Arachnoiditis of the brain is a rare diagnosis. Visible only on MRI of the brain with contrast as enhancement of the basal cisterns.
MRI of the brain. T1-weighted axial MRI with contrast. Arachnoiditis.
Viral encephalitis
Encephalitis is a diffuse parenchymal inflammation of the brain. Etiology - the disease can be caused by herpes infection, arboviruses, enteroviruses, echoviruses. Herpes is the most common cause of encephalitis. In adults, 95% of cases of herpes infection are caused by the herpes simplex virus type 1, in children by the herpes simplex virus type 2. In children, herpes is a primary infection, in adults it is the reactivation of latent viruses that enter the brain hematogenously or along the trigeminal and olfactory nerves . The frequency in adults is about 3 per 100 thousand or 10-20% of all viral encephalitis. Isolated sporadic cases are observed in newborns. Clinic: headache, fever, additionally – mental disorders, aphasia, convulsions, paresthesia, meningeal signs. The mortality rate for untreated herpetic encephalitis type 1 reaches 70%, with effective treatment - 30%; with untreated type 2 - 15% (local) - 60% (disseminated).
CSF cultures are positive in less than 5%. Antibodies appear in the blood only after 1-3 weeks. Therefore, the standard is a DNA test (after 24 hours) and a trial treatment with acyclovir.
CT and MRI of the brain reveal encephalitis no earlier than 3-5 days. Early signs consist of low-density fields in one or both temporal lobes on CT and hyperintensity in the same areas on T2-dependent MRI. MRI of the brain may show involvement of the lower frontal lobe and insula. Later, foci of hemorrhage appear, identified on T1-weighted MRI of the brain and a spotty type of enhancement on MRI of the brain with contrast.
| MRI of the brain. T2-weighted axial MRI. Herpetic encephalitis. | MRI of the brain. T1-weighted axial MRI after contrast. Herpetic encephalitis. |
Demyelinating diseases
Demyelinating diseases are a group of diseases, the main symptom of which is the destruction of the myelin sheaths of the nerves. In the popular MRI section there is a special article dedicated to MRI of multiple sclerosis. Many demyelinating diseases affect not only the brain, but also the spinal cord; MRI of the spinal cord in infectious diseases is described in a special section.
Acute disseminated encephalomyelitis
Acute disseminated encephalomyelitis (post-infectious encephalitis) is an autoimmune disease that occurs after a viral infection or vaccination (3-6% of cases). The pathophysiology of ADEM closely resembles the early stages of multiple sclerosis. Currently, ADEM is considered an acute demyelinating process. A variant is hyperacute hemorrhagic ADEM. The frequency is about 1 in 100 thousand. The age of patients in 80% of cases is under 10 years. The latent period is from 2 to 20 days. Clinic: acute onset in the form of fever, impaired consciousness, lethargy, convulsions (25%), may be optic neuritis, hemiparesis and ataxia. Laboratory tests are nonspecific. Mortality reaches 10-30%. In other cases, complete recovery.
On CT, in 50% of cases, subcortical areas of low density are detected, which may have a ring type of contrast. The sensitivity of brain MRI is 80-90%, and in some patients, changes are detected only a month after the onset of symptoms. MRI features consist of multiple hyperintense lesions on T2-dependent MRI images, they are asymmetrical, often confluent. There are hemorrhages into the lesions. The localization of foci can be any. A characteristic sign of ADEM is the disappearance of lesions on MRI of the brain as the patient recovers.
Proton density MRI. ODEM. The lesions are indicated by arrows.
Multiple sclerosis
Multiple sclerosis is an autoimmune demyelinating disease of the central nervous system. The process consists of local myelin destruction, axonal damage, gliosis and plaque formation. The frequency is about 2 per 1000 population. The M:F ratio is 1:2. The age can be any (2-74 years according to the literature), the peak falls on the young (average 35 years). Several variants of the course of MS are known. It is usually undulating, with progressive neurological deficits from relapse to relapse. Clinical signs consist of sensory and motor disturbances, visual disturbances and pelvic disturbances (80%). Different authors have proposed different criteria for multiple sclerosis, all of which include the presence of several (from 2 to 9) lesions typically located on MRI. The McDonald 2010 criteria were adopted by the International Committee for the Diagnosis of MS - they include the spatial distribution of lesions and dynamics over time. Spatial - 1 or more lesions on T2 in at least 2 of 4 zones: periventricular, subcortical, infratentorial or spinal cord. Temporary: new lesions appear on T2 or contrast-enhanced T1 MRI, simultaneous presence of asymptomatic contrast-enhancing or non-contrast lesions. Criteria for primary progressive MS: disease progression over the course of a year + 2 of three criteria – at least 1 lesion in a typical area, 2 or more lesions in the spinal cord, positive CSF test.
The sensitivity of CT even in clinically obvious MS is less than 50%, and increases slightly with a triple dose of contrast. The sensitivity and specificity of MRI in the early stages is 70-80%. The lesions are hyperintense on T2-weighted and proton density images. On T1-dependent MRI, only “old” lesions are visible. The localization of lesions can be any, but typical is the lower third of the corpus callosum, periventricular, in the trunk and spinal cord. The shape of the lesions is typically round and ovoid, directed radially from the ventricles on sagittal MR (finger or Dawson sign), reflecting a perivenular process. The edges of active lesions are blurred, there is weak contrast (often ring-shaped or C-shaped), which becomes more obvious with increasing dose. A slight mass effect has been described in aggressive cases (Marburg variant). The concentric variant of multiple sclerosis (Baló variant) is distinguished by the large size of the lesion, slight swelling around it and a circular structure. Cystic lesions are extremely rare in multiple sclerosis. The administration of hormones in doses significantly exceeding the physiological needs of the body causes inhibition of proliferative inflammatory processes. However, corticosteroid therapy slows astrocytic gliosis and the cavities remain unfilled.
On diffusion-weighted images, the signal from plaques is increased, the ICD is also increased, but in active plaques it may be reduced.
MRI of the brain. Axial and coronal MRI, reflecting proton density, and FLAIR type. Typical lesions of multiple sclerosis.
MRI of the brain with contrast. Parenchymal (left) and ring (right) types of contrast enhancement for multiple sclerosis.
MRI of the brain. Cystic lesions of multiple sclerosis. FLAIR and T1-dependent MRI with contrast.
MRI of the brain. Multiple sclerosis lesion on diffusion-weighted MRI (left) and diffusion map (right).
Often the first manifestation of multiple sclerosis is optic neuritis. Optic neuritis is a clinical diagnosis when vision is acutely impaired and there is pain. Isolated lesions in the optic nerve may not be accompanied by lesions in the brain, or they appear later (even after 15 years), or do not appear at all.
MRI of the brain. Optic neuritis in multiple sclerosis. T1-dependent MRI with contrast - enhancement of the intracanalicular part of the optic nerve on the left.
You can read about MRI of multiple sclerosis and other demyelinations in a separate article on this site.
Differential diagnosis of multiple sclerosis lesions should be carried out with other diseases manifested by focal changes:
- Other demyelinations
- Migraine foci
- Vasculitis (Systemic lupus erythematosus, etc.)
- Behçet's disease
- Lymphoma of the central nervous system
- Anti-phospholipid syndrome
- Infections (borelliosis, sarcoidosis, syphilis, AIDS, etc.)
- Ischemic changes
- Metabolic disorders
Proton density MRI of the brain. Migraine lesions (arrows).
MRI of the brain. Axial MRI type FLAIR. Lesions of systemic lupus erythematosus (arrows).
Progressive multifocal leukoencephalopathy
Progressive multifocal leukoencephalopathy (PML) is a demyelinating disease of viral etiology that develops against the background of immunodeficiency. Etiology – caused by JC viruses from the papovavirus group; this is the reactivation of a latent infection against the background of immunodeficiency. The virus infects oligodendrocytes and destroys them, which leads to demyelination. The clinical picture consists of a local neurological deficit and impaired consciousness. Death occurs within 9 months from the onset of the disease.
On MRI of the brain, PML lesions are often bilateral, asymmetrical, and rapidly increase in size. In 1/3 the posterior cranial fossa is affected, in 10% of cases the posterior cranial fossa is isolated. There are multiple foci. The basal ganglia are often involved. Enhancement on contrast-enhanced MRI is rare and, when observed, is peripheral and weak.
MRI of the brain. MRI type FLAIR. PML. Confluent lesion in the left frontal and parietal lobes.
Infantile ataxia with central hypomyelination
An extremely rare variant of demyelination (“vanishing” white matter disease) is observed in children after infections or minor injuries. The etiology is unknown; perhaps a gene defect plays a major role. The white matter is affected mainly in the periventricular zones with microcystic degeneration and destruction of the fibers of the corpus callosum. The clinical picture is represented by a lag in psychomotor development, spasticity, cerebellar ataxia, and visual impairment. MRI of the brain reveals symmetrical confluent lesions in the white matter. On T2-weighted MRI they have CSF signal intensity. A feature of the course of the disease is a gradual improvement in clinical symptoms and a decrease in lesions on MRI of the brain. Unlike other demyelinations, MRI of the brain shows cerebellar atrophy and significant spread of white matter lesions, down to the subcortical areas. Differential diagnosis is more carried out with dysmyelogenous diseases, especially leukodystrophies, in which a similar picture is observed on T2-weighted MRI of the brain.
MRI of the brain. T2-weighted axial MRI. Vanishing white matter disease.
Granulomatous inflammation
Tuberculosis
Neurotuberculosis is a consequence of hematogenous introduction of mycobacteria from the primary focus to the brain. Inflammation begins with subpial or subependymal cortical granulomas. The consequence of granulomatous inflammation is basal leptomeningitis, hydrocephalus, and small infarcts in the area of the subcortical nuclei. Parenchymal damage manifests itself in the form of tuberculomas, abscesses and cerebritis. Clinical manifestations consist of low-grade fever, headaches, and sometimes seizures.
CT scan reveals infarcts, contrast enhancement of membranes and tuberculomas. Tuberculomas become calcified and look like “targets”.
On MRI of the brain, tuberculomas are typically hypointense, but can also be hyperintense and surrounded by edema. Signal enhancement on T1-weighted MRIs on contrast-enhanced MRI is homogeneous or ring-shaped (with calcification). Cerebritis and meningitis appear nonspecific.
CT. Neurotuberculosis. Foci of cerebral infarction.
MRI of the brain. Axial T2-weighted MRI. Neurotuberculosis. Tuburculoma.
Sarcoidosis
The pathological anatomy of sarcoidosis is very similar to tuberculosis. Brain damage is observed in 5% of patients with sarcoidosis. Neurosarcoidosis occurs in the form of leptomeningitis and parenchymal lesions.
On CT and MRI, sarcoids, unlike tuberculomas, do not have a calcified center. The localization of sarcoids on MRI of the brain can be any, but the typical hypothalamus and optic chiasm.
MRI of the brain. T1-dependent MRI with contrast. Neurosarcoidosis. Damage to the membranes, cranial nerves, lesions in the trunk (arrows).
Acquired immunodeficiency syndrome
The disease is caused by HIV viruses. Neurological disorders are observed in more than 80% of patients, and in approximately 10% they are the first manifestations. It is necessary to distinguish between the signs of HIV infection itself and the symptoms of layered (opportunistic) infection - cytomegalovirus, cryptococcosis, toxoplasmosis, tuberculosis, syphilis, PML or layered tumors - lymphoma and Kaposi's sarcoma. At the earliest stages of HIV infection, CT and MRI do not detect pathology. As it progresses, MRI of the brain in AIDS shows that the subcortical gray matter is affected - the dementia complex, and then damage to the white matter develops - atrophy and leukoencephalopathy.
MRI of the brain. Axial T1-weighted MRI with contrast. Dementia due to HIV infection: atrophy and leukoencephalopathy.
Toxoplasmosis is the most common infection associated with AIDS. Toxoplasmosis in AIDS is a reactivation of the infection.
CT and MRI of the brain show multiple nodular or ring-shaped lesions surrounded by vasogenic edema of varying severity. Most often, MRI lesions are found at the border of the white and gray matter, the basal ganglia and the thalamus opticum.
MRI of the brain. Axial T2-dependent MRI. Toxoplasmosis.
Cryptococcosis - occurs as an independent infection, as well as as an opportunistic infection in 6-7% of AIDS patients. It is a fungal infection and in AIDS occurs in the parenchymal form. Cysts, pseudocysts and multiple hyperintense foci are detected on T2-dependent MRI of the brain. Leptomeningitis does not always enhance on contrast-enhanced MRI. The choroid plexuses are dilated (plexitis). Other mycoses also occur with AIDS: candidiasis and coccidioidomycosis.
MRI of the brain. Axial T1-dependent MRI with contrast. Cryptococcosis. Lesions and leptomeningitis.
Cytomegalovirus infection occurs in the form of encephalitis and ventriculitis. Bilateral lesions with characteristic localization in semi-oval centers are identified.
MRI in St. Petersburg in leading centers; for any questions, please contact the administrator by phone. 676-66-48. When examining in an open MRI, there is no fear of confined space, but the examination takes a little longer.
Leave feedback.
10/06/2016 Added by Sergey
MRI in St. Petersburg, USA
Great article. Thank you. MRI doctor.
business 0.3 MRI in St. Petersburg, USA 5.0 5.0 1 1 Excellent article.
Thank you. MRI doctor. MRI in St. Petersburg USA
Treatment of brain abscess
When treating a brain abscess, two types of treatment can be used together or separately:
- Drug treatment involves the use of antibacterial and anti-inflammatory drugs.
- Surgical treatment - in the last stages of abscess development, the lesion is cut, removing purulent formations and treating the cavity with an antibiotic.
- Detoxification of the body to eliminate the effects of an abscess and prevent its development again.
- General restorative therapy that provides the patient with a full recovery.
- Elimination of functional disorders that appear as a result of severe disease.
Encephalitis
Pathogenetic therapy Oral and parenteral administration of fluid is carried out, taking into account the water-electrolyte balance and acid-base state. In severe cases of the disease, glucocorticoids are used. If the patient does not have bulbar disorders or disorders of consciousness, then prednisolone is used in tablets at the rate of 1.5-2 mg/kg per day. The drug is prescribed in equal doses in 4-6 doses over 5-6 days, then the dosage is gradually reduced (the total course of treatment is 10-14 days). For bulbar disorders and disorders of consciousness, prednisolone is administered parenterally at a rate of 6-8 mg/kg. Lumbar puncture is contraindicated. To combat hypoxia, humidified oxygen is administered through nasal catheters (20-30 minutes every hour), hyperbaric oxygenation will be performed (10 sessions at a pressure of p 02-0.25 MPa), sodium hydroxybutyrate will also be administered intravenously at 50 mg/kg per day or Seduxen 20-30 mg per day.
Indications. Allergic reactions, blood transfusion shock, anaphylactic shock, anaphylactoid reactions, cerebral edema, bronchial asthma, status asthmaticus, acute hepatitis, hepatic coma.
Contraindications. Hypersensitivity, previous arthroplasty, pathological bleeding, transarticular bone fracture, aseptic necrosis of the epiphyses of the bones that form the joint. Carefully. Parasitic and infectious diseases of a viral, fungal or bacterial nature: herpes simplex, chicken pox, measles; amebiasis, strongyloidiasis (established or suspected); systemic mycosis; active and latent tuberculosis, gastric and duodenal ulcers, esophagitis, gastritis, acute or latent peptic ulcers, diverticulitis, arterial hypertension, hyperlipidemia, diabetes mellitus, severe chronic renal and/or liver failure, nephrourolithiasis.
Side effects. Nausea, vomiting, increased or decreased appetite, bradycardia, insomnia, dizziness.
Also, in the treatment of encephalitis, diuretics are used to dehydrate and combat edema and swelling of the brain (10-20% solution of mannitol 1-1.5 g/kg intravenously; furosemide 20-40 mg intravenously or intramuscularly, 30% glycerol 1-1 .5 g/kg orally, diacarb, brinaldix).
Indications. Cerebral edema, hypertension, acute renal failure, epilepsy, Meniere's disease, glaucoma, gout.
Contraindications. Hypersensitivity, acute renal failure, liver failure, hypokalemia, acidosis, hypocortisolism, Addison's disease, uremia, diabetes mellitus, pregnancy (first trimester), nephritis, hypochloremia, hemorrhagic stroke.
Side effects. Hypokalemia, myasthenia gravis, convulsions, dehydration, tachycardia, nausea, vomiting.
A number of Russian pharmacologists and clinicians claim the existence of a highly effective antiviral drug, yodantipirin. It is stated that it has an etiotropic effect against flavivirus infection, but it should be noted that this drug is not used anywhere in the world for antiviral purposes, and there is no reliable data from evidence-based medicine confirming its clinical effectiveness.
Indications: Tick-borne encephalitis (treatment and prevention in adults). Contraindications: Hypersensitivity, hyperfunction of the thyroid gland. Side effects: Allergic reactions, swelling, nausea.
Etiotropic therapy Etiotropic therapy consists of prescribing homologous gamma globulin titrated against tick-borne encephalitis virus. The drug has a clear therapeutic effect, especially in moderate and severe cases of the disease. Gamma globulin is recommended to be administered 6 ml intramuscularly, daily for 3 days. The therapeutic effect occurs 12-24 hours after its administration: body temperature decreases, the patient's condition improves, headaches and meningeal symptoms decrease. The sooner gamma globulin is administered, the faster the therapeutic effect occurs. In recent years, serum immunoglobulin and homologous polyglobulin, which are obtained from the blood plasma of donors living in natural foci of tick-borne encephalitis, have been used to treat tick-borne encephalitis. On the first day of treatment, serum immunoglobulin is recommended to be administered 2 times at intervals of 10-12 hours, 3 ml for mild cases, 6 ml for moderate cases and 12 ml for severe cases. In the next 2 days, the drug is prescribed 3 ml once intramuscularly. Homologous polyglobulin is administered intravenously at 60-100 ml. It is believed that antibodies neutralize the virus, protect the cell from the virus by binding to its surface membrane receptors, and neutralize the virus inside the cell, penetrating it by binding to cytoplasmic receptors.
Antiviral drugs are also used - nucleases that inhibit the replication of the virus. RNase is used intramuscularly in an isotonic solution, 30 mg 5-6 times a day. Per course - 800-1000 mg of the drug. The antiviral effect is exerted by the drug cytosine arabinose, which is administered intravenously for 4-5 days at the rate of 2-3 mg per 1 kg of body weight per day.
Infusion therapy In case of severe symptoms of intoxication, infusion therapy is carried out. For cerebral edema and bulbar disorders, the most rapid effect is provided by intravenous administration of prednisolone (2-5 mg/kg) or dexazone, hydrocortisone. For psychomotor agitation, epileptic seizures, seduxen is administered intravenously or intramuscularly - 0.3-0.4 mg/kg, sodium hydroxybutyrate - 50-100 mg/kg, droperidol - from 0.5 to 6-8 ml, hexenal - 10% solution 0.5 ml/kg (with preliminary administration of atropine); in enemas - chloral hydrate 2% solution 50-100 ml.
The complex of therapy should include antihistamines - calcium chloride solution, diphenhydramine, diprazine, pipolfen or suprastin, B vitamins, especially B6 and B12, ATP. With the development of flaccid paresis, the use of dibazole, galantamine, prozerin, oxazil is indicated.
Symptomatic therapy - Antipyretic drugs - Anti-inflammatory (glucocorticoids) - Anticonvulsant therapy (benzonal, difenin, finlepsin) - Detoxification therapy (saline solutions, protein drugs, plasma substitutes) - Resuscitation measures (ventilators, cardiotropic drugs) - Prevention of secondary bacterial complications (broad-spectrum antibiotics actions)
Rehabilitation treatment After discharge from the hospital, in the presence of neurological disorders, a course of rehabilitation treatment is carried out. Patients may be prescribed B vitamins, aloe extract, Cerebrolysin (contraindicated in the presence of seizures), aminalon, piracetam, pyriditol, pantogam.
Treatment of parkinsonism . An effective treatment for parkinsonism is taking L-DOPA (a dopamine precursor). The drug penetrates the blood-brain barrier and compensates for the lack of dopamine in the basal ganglia.
The most effective is combination treatment, which allows you to equalize the balance by strengthening the dopaminergic system (using L-DOPA or L-DOPA-containing drugs and meditane) and suppressing the cholinergic system (using cyclodol).
Treatment with L-DOPA is carried out according to a specific scheme, which involves gradually increasing the dosage and amount of the drug over several weeks. To reduce irritation of the walls of the gastrointestinal tract, the drug is prescribed after meals. The initial dose is 0.125 g per day, with a gradual increase by 0.125-0.25 g per day. The therapeutic effect is observed at different dosages, usually from 2 g to 5-6 g per day. With prolonged use of the drug over many years, its effectiveness decreases.
Contraindications to such treatment are bleeding stomach ulcers, severe liver and kidney diseases, decompensated state of the cardiovascular system, gloucoma, and mental illness. Positive results from the use of L-DOPA or its derivatives are observed in approximately 70% of patients. Some of them return to work.
Treatment of hyperkinesis . Metabolic drugs, α-blockers, neuroleptics (haloperidol, chlorpromazine) and tranquilizers are prescribed.
Treatment of Kozhevnikov epilepsy . Metabolic drugs, anticonvulsants (Depakine, Tegretol, Sereysky mixture), tranquilizers (Elenium, meprobamate, trioxazine, gindarine, mebikar) and antipsychotics (aminazine) are also prescribed.