Home / Neurologist / Cerebrovascular diseases
Diseases of the cerebral vessels , unfortunately, are now not at all uncommon. In Russian practice, vascular diseases of the brain are called discirculatory encephalopathy, and in foreign practice - ischemic brain disease. All these names describe the same condition.
Discirculatory encephalopathy (DE) is a condition manifested by a progressive multifocal disorder of brain function caused by cerebral circulatory insufficiency. The progression of neurological and mental disorders can be caused by persistent and long-term cerebral circulatory failure. Of no small importance in this regard is the aging process of the nervous, respiratory, and cardiovascular systems, which also leads to the development or intensification of hypoxia (oxygen starvation) of the brain. Brain hypoxia itself leads to further damage to the mechanisms regulating cerebral circulation. This fully applies to DE - a consequence of chronic vascular insufficiency of the brain, causing changes in brain tissue and disruption of its functioning.
According to statistics, up to 85% of the population are predisposed to developing various diseases related to the blood supply to the brain. This frightening number is due to the lifestyle of modern man. Many people know the word “hypertension” and “VSD” from adolescence, only if at school the diagnosis of “heart disease” was a reason not to go to physical education, then in adulthood a person receives real manifestations and evidence of the diagnosis.
About 30% of the population has a hereditary predisposition to stroke. 25% of stroke survivors die almost immediately (usually elderly people), another 25% die within six months; the risk of recurrent stroke over the next 1-2 years is 60%.
Symptoms of cerebral atherosclerosis
Unfortunately, cerebral atherosclerosis may not manifest itself for years. Only regular examination and monitoring of blood sugar and lipid levels helps to recognize the impending danger in time and take effective measures.
Entrust your health to the professionals of the multifunctional center of the FMBA of Russia with extensive experience in the treatment of patients with vascular pathology, as well as prevention and subsequent recovery. Annual monitoring of your health will help you prevent vascular accidents in time and maintain a high quality of life for many years.
Below is Table 1 with the most common symptoms of cerebral atherosclerosis at different stages of the disease. It will help you recognize the first signs of pathology and promptly seek medical help.
| Stage | Patient complaints |
| First stage | Often : headache, tinnitus, memory loss (remembers the past well, but cannot remember new information. Often : asthenia - fatigue, weakness, inattention, general lethargy. Relief may occur after rest. Rarely : sleep disturbance, insomnia or daytime sleepiness. |
| Second stage | Disease progression . Anxiety, suspiciousness, mood swings, and a tendency toward depression appear. Memory loss: a person does not remember what happened today and stops thinking clearly and logically. Headache and tinnitus become constant. Speech: unclear, diction changes. Tremors of the limbs and head appear. Vision and hearing deteriorate. Coordination in space deteriorates: dizziness and unsteadiness of gait are bothersome. There may be a loss of sensitivity in one half of the body and the appearance of facial asymmetry. |
| Third stage (irreversible) | Dementia develops . The patient may behave like a child or become whiny and aggressive. Not interested in the world around him and the events in it. Not oriented in space and time. There is complete or partial memory loss. Needs constant care because he has lost self-care skills at home. |
Such complaints may indicate that the lumen of an important vessel in the brain is closed by more than 50%. Be attentive to your health!
Self-medication of cerebral atherosclerosis is not acceptable!
Even at the first stage! As we said above, the first symptoms of the disease appear already with a significant degree of vascular damage.
Entrust your health to specialists with many years of experience in the treatment of vascular accidents and subsequent neurorehabilitation. Start by seeing a neurologist and tell him about how you have been feeling over the past months.
A professional, sensitive attitude towards patients and attention to detail will allow us to recognize and prevent irreversible changes in the brain in time.
Vascular stenosis
Atherosclerosis
Diabetes
Ulcer
2937 12 August
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Vascular stenosis: causes, symptoms, diagnosis and treatment methods.
Definition
Vascular stenosis (Greek στενός - “narrow, cramped”) is a partial or complete persistent narrowing of the lumen of blood vessels with limitation or complete cessation of blood flow.
Causes of vascular stenosis
Depending on which vessels are affected, a distinction is made between stenosis of arterial vessels (aorta, arteries, arterioles) and stenosis of venous vessels (superior vena cava, inferior vena cava, veins, venules).
Vascular stenosis can be either congenital or acquired.
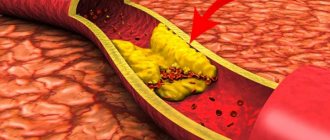
The main cause of acquired stenosis of the aorta, arteries of the lower extremities, and coronary arteries of the heart is atherosclerosis, a systemic metabolic disease with predominant damage to the vascular wall. The degree of narrowing of the artery and its length may vary. When blood pressure increases, the sclerotic inner layer of the vessel (endothelium) is easily damaged, as a result, the blood clotting process is activated and a blood clot is formed.
Blockage of the vessel can lead to ischemia or necrosis of the tissue or organ.
Risk factors for the development of atherosclerosis include:
- male gender;
- elderly age;
- smoking;
- dyslipidemia (violation of the normal ratio of blood lipids);
- diabetes,
- arterial hypertension,
- increased blood homocysteine;
- elevated levels of C-reactive protein (CRP);
- increased blood viscosity and hypercoagulable states;
- chronic renal failure.
Another disease leading to arterial stenosis is obliterating endarteritis (spontaneous gangrene) - a chronic disease of peripheral blood vessels (mainly affecting the arteries of the feet and legs).
Mostly men under the age of 25-40 are affected. Those at risk include smokers, as well as people with frostbite on their feet. Diabetic angiopathy, characterized by damage to both small vessels and large and medium-sized arteries, develops in patients with diabetes mellitus. In diabetic macroangiopathy, when large blood vessels are affected, changes characteristic of obliterating atherosclerosis are found in the wall of the great vessels. With microangiopathies, when small blood vessels are affected, thickening of the walls of microvasculature vessels (arterioles, capillaries, venules) occurs, which leads to a narrowing of the lumen and deterioration of the blood supply to organs and tissues.
Coarctation of the aorta (congenital segmental narrowing of part of the aorta that obstructs blood flow) occurs as a result of improper fusion of the aortic arches in the embryonic period. The length of the narrowing is usually 1-2 cm. The ascending aorta and branches of the aortic arch expand, their diameter increases significantly, and the walls of the arteries participating in the collateral circulation become thinner. Two modes of blood circulation are formed in the systemic circle: up to the point of obstruction to blood flow there is arterial hypertension, and distal (or below) there is hypotension.
Venous stenosis most often occurs as a result of direct damage to the vascular wall during catheter insertion and is then aggravated by the constant presence of a foreign body and mechanical irritation. Inflammation and activation of the blood coagulation system are observed in the vessel wall. These changes lead to proliferation (multiplication) of smooth muscle cells, thickening of the vein wall, and the formation of microthrombi.
Thus, risk factors for the development of central venous stenosis are: the use of a central venous catheter, infections associated with the installation of a catheter, and concomitant diseases.
Systemic vasculitis, tumor diseases and other causes of vascular stenosis are detected much less frequently.
Classification of the disease
According to the type of blood vessels:
- arterial stenosis;
- venous stenosis
Due to the occurrence:
- congenital;
- acquired.
By localization:
- Stenosis of the arteries of the lower extremities.
- Stenosis of the carotid (carotid) and cerebral arteries.
- Stenoses of the arteries of internal organs:
- renal arteries,
- mesenteric arteries etc.
- Aortic stenosis.
- Stenosis of coronary vessels.
By caliber of damage:
- stenosis of large vessels (aorta and its branches);
- stenosis of medium-diameter vessels;
- stenosis of small vessels (arterioles and capillaries).
Symptoms of vascular stenosis
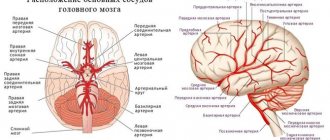
Damage to the blood vessels of the brain is one of the main causes of mortality and disability in the population. 2/3 of ischemic strokes are associated with narrowing and deformation of the carotid arteries.
The risk of developing ischemic stroke is directly related to the degree of narrowing of the artery lumen.
Occlusion (closure) of the internal carotid artery leads to the development of stroke in 40% of cases.
Damages to the blood vessels of the brain can occur in several forms:
- The asymptomatic form is characterized by the absence of focal and cerebral neurological symptoms (impaired consciousness, headache, vomiting, slow pulse).
- Discirculatory encephalopathy is characterized by a predominance of general cerebral symptoms; focal neurological symptoms are absent or appear in a very mild form.
- Transient ischemic attacks manifest themselves in the form of transient disorders of cerebral circulation of the ischemic type and are accompanied by the appearance of focal neurological symptoms that resolve within 24 hours.
- The consequences of a minor stroke are an acute ischemic cerebrovascular accident with the development of neurological symptoms, which almost completely regress within a month as a result of conservative therapy.
- The consequences of a completed stroke are an acute ischemic disorder of cerebral circulation, accompanied by the development of persistent focal neurological and cerebral symptoms.
- Ischemic stroke is damage to brain tissue with disruption of its functions due to obstruction or cessation of blood flow.
Atheroslerotic lesion of the coronary arteries of the heart is manifested by angina pain, but can sometimes be perceived by the patient as discomfort, a feeling of heaviness, compression, tightness, distension, burning or lack of air.
Most often, the pain is localized behind the sternum or along the left edge of the sternum; it can radiate (give) to the neck, lower jaw, teeth, interscapular space, and less often to the elbow or wrist joints, mastoid processes. Pain with angina pectoris usually lasts from 1 to 15 minutes. Occurs during significant physical or emotional stress. After taking nitroglycerin or stopping the exercise, the pain stops. As angina progresses, an attack may occur with minimal exertion and then at rest.
The main symptom of renal artery stenosis is a persistent increase in blood pressure, which is difficult to respond to drug therapy. Approximately 90% of cases of renal artery stenosis are caused by atherosclerosis; in 10% of cases, stenosis occurs due to fibromuscular dysplasia, a group of diseases that affect the walls of the arterial vessel.
With renal artery stenosis, the blood supply to the kidney tissue is reduced, hormonal factors (renin-angiotensin-aldosterone system) that regulate blood volume and blood pressure are activated, and the development of chronic kidney disease is accelerated.
Stenosing damage to the vessels supplying blood to the abdominal organs (mesenteric arteries) is more often observed in middle-aged and elderly people and manifests itself as chronic abdominal ischemia syndrome, so the main complaint of patients is pain, which appears after 20-25 minutes. after eating, lasts 1-2 hours and usually subsides on its own. The pain can be localized in the epigastric region, directly under the xiphoid process, and radiate to the right hypochondrium or spread from the periumbilical region throughout the abdomen. Some patients note a feeling of constant heaviness in the abdomen, and vomiting is rarely observed.
Other symptoms of chronic abdominal ischemia are intestinal dysfunction, expressed by disturbances in its motor, secretory, absorption functions, and progressive weight loss.
Obliterating atherosclerosis of the aorta and main arteries of the lower extremities is more common in men over 40 years of age and deprives them of their ability to work. The process can be localized in large vessels (aorta, iliac arteries) or medium-sized arteries (femoral, popliteal).
Small atherosclerotic lesions of the arteries of the lower extremities may not be clinically manifest. With continued vasoconstriction, intermittent claudication occurs, which is manifested by discomfort or pain in the muscles of the lower limb during physical activity. Damage to the terminal aorta and iliac arteries can cause pain in the buttocks, thigh, and calf. Impaired patency of the femoral-popliteal segment is characterized by pain in the calf. Occlusion of the arteries of the leg usually causes pain in the calf, foot, absence or decrease in skin sensitivity in them.
With obliterating endarteritis, trophic disorders are observed (cracks, dry skin, brittle nails, ulcers), intermittent claudication, leg pain, necrosis and gangrene of the limb.
In the generalized form of obliterating endarteritis or atherosclerosis, not only the vessels of the extremities are affected, but the visceral branches of the abdominal aorta, branches of the aortic arch, cerebral and coronary arteries.
The clinical picture of diabetic macroangiopathy consists of the clinical picture of microangiopathy and atherosclerosis of the great vessels, but is characterized by a more severe and progressive course, often ending in gangrene.
The clinical picture of diabetic microangiopathy of the lower extremities is similar to that of obliterating endarteritis.
With coarctation of the aorta, symptoms depend on the severity of the disease. In the case of significant narrowing of the aorta, the parents of the newborn pay attention to the pale skin, sweating, and difficulty breathing of the child. In older children and adults, the symptoms are usually mild: high blood pressure, headache, cold extremities, nosebleeds.
Stenosis of the central veins is clinically manifested by swelling of the extremities, pain in them and trophic changes (cyanosis, thinning of the skin, cracks, ulcers, etc.).
Diagnosis of vascular stenosis
Diagnosis of the disease is based on the analysis of patient complaints, medical history data, clinical picture, data from laboratory and instrumental research methods.
To clarify the cause of vascular stenosis, the following may be recommended:
- clinical blood test: general analysis, leukoformula, ESR (with microscopy of a blood smear in the presence of pathological changes);
Diagnostics
A neurologist deals with cerebral atherosclerosis. His task is to collect anamnesis, as well as conduct a series of tests. Doctor:
- will ask you to look up (a sick person will not be able to fulfill the request);
- will check the reflexes (they will be either excessively high or low, and asymmetrically);
- will ask you to stretch your arms forward and look to see if there is any tremors in the fingers, or if the patient is losing balance;
- will ask you to touch your nose with the tip of your finger with your eyes closed (the patient will not be able to cope with this task).
This is only a small component for assessing the patient’s health. Therefore, more detailed examinations are required next:
- consultation with an ENT doctor, ophthalmologist and other specialists depending on the identified disorders;
- biochemical blood test for triglycerides and cholesterol (lipid spectrum);
- According to indications, instrumental examinations are carried out.
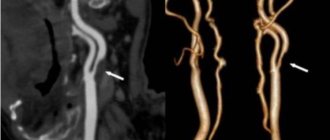
To assess the condition of cerebral vessels, the following is carried out:
- Ultrasound of the brain and neck using two-dimensional and transcranial duplex scanning technology;
- angiography of cerebral vessels;
- Doppler ultrasound;
- MRI of the brain in vascular mode;
- REG (radioencephalogram);
- CT computed tomography of the brain and blood vessels;
- EEG – electroencephalogram.
The diagnostic capabilities of our multifunctional center of the FMBA of Russia allow us to carry out not only these, but also any other examinations necessary for the patient using the most modern and accurate equipment. You will be able to get advice from related specialists on any clinical case, including suspected cerebral atherosclerosis.
Diagnostic procedures
Vascular diseases of the brain are dangerous and require diagnostics in medical institutions. The procedures help to identify emerging pathology at the primary stages. After a detailed study of the etiological picture, the patient is referred to a specific doctor.
The specialist determines the feasibility of carrying out specific types of diagnostics and may prescribe one or a set of tests: MRI, duplex examination, administration of a contrast agent for tomography, blood tests and other biological materials.
Such examinations make it possible to identify the cause of spasms and problems with the functioning of cerebral vessels, and determine the course of treatment for a particular patient. In everyday conditions, such diagnostics are difficult to carry out. Therefore, going to the hospital should not be ignored if suspicious signs appear.
Treatment of cerebral atherosclerosis
It is not only the neurologist who treats patients with atherosclerosis in our center. We treat the disease comprehensively with the involvement of doctors from different specialties. This approach makes the recovery process comfortable, gives better results and helps patients return to their normal lives sooner.
The basis for the treatment of cerebral atherosclerosis is the correct selection of nutrition. On the one hand, the diet combines a complete diet with individually designed physical activity. On the other hand, medications help compensate for the pathological process and reduce the harmful effects of the disease on the body.
Medicines used:
- diuretics;
- drugs that normalize lipid and blood sugar levels;
- vitamins;
- drugs to improve cerebral circulation;
- means for normalizing blood pressure and heart rate;
- thrombolytic agents, etc.
Types and classification of vasculitis
Vasculitis is divided into types:
- primary;
- secondary;
- systemic.
In the first case, we are talking about an independent and still just beginning disease. The second type may appear with other pathologies, for example, tumors. It can also occur as a reaction to an infection. Systemic vasculitis can occur in different ways. It leads to inflammation of blood vessels and damage to their walls, and tissue necrosis cannot be ruled out. Without proper treatment, complications usually occur, including death.
Based on the caliber of the affected vessels, a classification of vasculitis was identified. It may be in the form:
- arteritis (affects large vessels);
- phlebitis (affects the walls of the veins);
- arteriolitis (inflames the arteries and arterioles);
- capillaritis (affects capillaries).
Also included in a separate category is vasculopathy, which is characterized by the absence of clear signs of inflammation and infiltration of the vascular walls.
The degree of vascular damage can be mild, moderate and severe.
Prevention
Below are a few useful habits that will help significantly reduce the risk of developing atherosclerosis:
- to give up smoking;
- nutrition balanced in composition of nutrients;
- correction and maintenance of optimal body weight;
- annual preventive monitoring of lipid and blood sugar levels.
The diagnostic capabilities of our center allow us to establish a diagnosis quickly and accurately. Based on the results of the examination, you will be advised by experienced neurologists, whose knowledge has helped save hundreds of patients.
Also, individual health monitoring programs have been developed on the basis of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency of Russia.
- for men (under 40 years old, over 40 years old, standard);
- for women (under 40 years old, over 40 years old, standard based on age and optimal)
Don't put off taking care of your health. Call us or make an appointment to assess your risk of atherosclerosis and receive comprehensive recommendations.
Causes of the disease
The reasons for the formation of primary vasculitis are still unknown to science. Secondary disease can occur against the background of:
- acute or chronic infection;
- genetic (hereditary) predisposition;
- thermal effects (overheating or hypothermia of the body);
- various injuries;
- burns;
- contact with chemicals and poisons.
Another cause of vasculitis can be viral hepatitis. One or more risk factors are enough to change the antigenic structure of tissues. In this case, the immune system begins to secrete antibodies, which further damage the tissue, in this case the blood vessels. This leads to an autoimmune reaction and inflammatory and degenerative processes.