Irritation of the cortex covering the deep structures of the brain is a natural process that normally occurs as a result of exposure to external factors, which forces the central nervous system to react and form a physiological response. Pathologies of nervous structures provoke disturbances in the functioning of the brain, which is reflected in irritation (irritation) of its parts without the influence of external stimuli. This condition leads to malfunctions in all body systems. Diagnosed at any age, regardless of the person’s gender.
Definition of pathology
Irritative disorders arise due to disruption of the transmission of nerve impulses, which provokes a deterioration in brain activity. Irritation of the cortex covering the brain is a pathological condition that is manifested by the spontaneous appearance of a focus of irritation in a certain area, which leads to the appearance of characteristic symptoms. An example of a normal reaction of the nervous system to an external irritant is a decrease in pupil diameter in response to bright light, which occurs as a result of irritation of the optic nerve.
Spontaneous irritation without obvious reasons is a pathology that significantly complicates a person’s life. Irritation of areas of the brain is not included in the international list of diseases ICD-10, because more often irritation of the cortical, median (deep), diencephalic structures is a symptom of the primary disease. Among the pathologies manifested by similar symptoms, it is worth noting a tumor localized in the brain tissue, organic damage to the nervous tissue of various etiologies.
There are focal (irritation of a local area of the cortex) and diffuse (pathological process spreads throughout the entire cortex) irritation of cortical structures. The pathological condition may be accompanied by specific symptoms or be asymptomatic. Irritation of stem structures, which include the trunk, mediobasal and intermediate sections, leads to dysfunction of the brain and body. Failures manifest themselves in the form of syndromes of neuropsychological and autonomic origin.
Irritation in the area of diencephalic structures, which includes the thalamus, hypothalamus, pituitary gland and other parts of the brain, is a pathological condition, often manifested by decreased self-esteem, sudden mood swings, apathy, and increased fatigue, which indicates behavioral and psycho-emotional disorders.
Symptoms
Signs of cortical irritation are determined by the localization of irritation. Symptoms are directly related to the area of the cortex where focal spontaneous irritation occurs:
- Frontal zone. Accompanied by the occurrence of motor reactions. Muscle contraction depends on the location of stimulation in the precentral frontal gyrus. After irritation of the frontal area, complex motor patterns may appear: the patient will begin to tie his shoelaces in the air.
- Temple area. Simple auditory hallucinations (acoasms) and complex hallucinations appear, accompanied by a voice commenting on the content.
- Occipital zone. Accompanied by simple (photopsia) and complex visual hallucinations. Photopsia are second-long hallucinations: flashes of light, a small spot. Complex hallucinations consist of images, the content of which is determined by the patient’s inner mental life.
- The parietal zone is an area of general sensitivity. Tingling, numbness, and crawling sensations occur in different parts of the body. Irritation in this area is also accompanied by perverted sensations of touch, pain, heat or cold.
Diffuse irritation of the cortex is accompanied by small (petit mal) and large (grand mal) convulsions.
Petite seizures include myoclonic spasms of individual muscles. Muscle contraction is characterized by rhythm and absence of complications. Petit mal also manifests itself as absence seizures – short-term loss of consciousness while maintaining muscle tone throughout the body. After 20-30 seconds of “switching off”, patients come to their senses and continue their work. They don't know that they just came out of consciousness.
Grand mal consists of several successive stages:
- Harbingers. The day before extensive seizures, people feel unwell and have a headache. They don't sleep well.
- Aura. Within 30-40 minutes, patients complain of vague pain in the abdomen, arm or heart.
- Tonic phase. The man loses consciousness and falls. All the muscles of the body contract simultaneously and synchronously. Skin color turns blue, breathing is uneven. Duration – no more than 60 seconds.
- Clonic phase. All muscles of the body contract unevenly, asynchronously, chaotically: each muscle contracts separately. Lasts 1-2 minutes.
In general, the entire grand mal seizure lasts up to 3 minutes. After the last phase, the muscles relax and the patient goes into deep sleep. After waking up, he experiences disorientation and retrograde amnesia (he does not remember what happened before the seizure).
Causes
The pathological condition can develop as a complication of somatic diseases - measles, chickenpox, rubella, malaria. Such disorders can be provoked by an increase in intracranial pressure due to various reasons. Reasons for irritative changes include:
- Traumatic brain injuries.
- Infectious diseases affecting parts of the brain (meningitis, encephalitis, abscess, arachnoiditis).
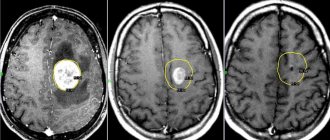
- Tumor processes and other space-occupying formations in the cranial cavity (cysts, foci of hemorrhage).
- Demyelinating diseases, including multiple sclerosis.
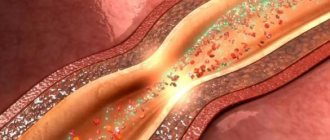
- Lesions of the vascular system supplying brain tissue (atherosclerosis, TIA - transient cerebrovascular accident, embolism - blockage of a vessel, ischemic, hemorrhagic strokes).
- Neurodegenerative diseases.
- Violation of metabolic processes.
- Intoxications occurring in acute and chronic forms (chronic alcoholism, chemical poisoning).
Among the provoking factors, it is worth noting alcohol abuse, drug use, stress, excessive mental, mental, physical stress, living in a region with an unfavorable environment. Often, such disorders occur during pregnancy, as a consequence of hormonal changes against the background of existing organic brain damage.
Diffuse changes in biopotentials and their symptoms
Disorders may occur in the brain and its individual parts, resulting in the development of autonomic, psychopathological and neuropsychological disorders. Irritation of the cerebral cortex and its parts is an irritation that occurs as a result of infectious processes, neoplasms, circulatory or metabolic disorders.
Signals are transmitted between neurons in the brain. This process is carried out using electrical impulses. When signal transmission is disrupted, it negatively affects the entire human body. At the same time, the bioelectrical activity of the brain deteriorates.
The presence of these failures can be determined using instrumental diagnostic methods. Disturbances in the bioelectrical activity of the brain indicate the development of pathological processes.
As a result of traumatic brain injury and under the influence of other factors, the activity of electrical impulses through which neurons transmit signals to each other decreases. This is called disorganization of bioelectrical activity.
As a result of injuries, diffuse irritation of the brain may occur. These are mild disorders that lead to minor disruptions in the transmission of impulses. If treatment is carried out, then within several months or years the condition of the stem structures of the meninges can be restored. Diffuse changes are spoken of when local disturbances cannot be detected.
Such deviations can manifest themselves as mood swings, fatigue, and discomfort.
Brain activity can be disrupted in different parts. When the cerebral cortex is damaged, epilepsy attacks and other disorders appear, which depend on the area of damage:
- If general cerebral disturbances of an irritative nature are observed behind the middle frontal part, then the head begins to twitch first, and gradually the symptom spreads to the whole body.
- When the adversive field is damaged, seizures appear on the side of the body opposite the irritated side of the brain. At the beginning of the attack, the patient may lose consciousness.
- Irritation of the opercular zone is accompanied by loss of control over chewing, slurping and swallowing movements.
- If the central gyrus is affected, the patient is bothered by epileptic seizures, the onset of which is observed on the face and limbs.
- An irritated posterior central gyrus is accompanied by numbness and tingling in half the body.
- When the occipital lobe is damaged, hallucinations appear, the head and eyes turn in the opposite direction, and a widespread seizure develops.
- The process of irritation in the cranial fossa causes trigeminal neuralgia, problems with hearing and vision, loss of smell, and changes in the sensitivity of the facial muscles.
Dysfunctions of mid-stem structures may occur. They are also called diencephalic. This process is also accompanied by the development of epileptic seizures. In this case, cognitive, emotional, speech and autonomic disorders are observed.
Irritation of the lower brainstem is accompanied by disturbances in consciousness, memory and attention, and changes in periods of sleep and wakefulness.
When irritation of the central part of the hypothalamus occurs, disorders develop in which:
- Autonomic dysfunctions occur, accompanied by negative emotions.
- Memory and attention deteriorate significantly.
- The manifestations of Korsakov's psychosis are disturbing. In this case, a person loses orientation in space, and false memories may appear.
WE RECOMMEND WATCHING: What causes gliosis changes in the brain
Cognitive and speech disorders with irritation of the thalamus are completely reversible.
EEG BEA shows that irritation can be considered irritation of the cortical and deep structures of the brain. Disorders develop as a secondary disorder, so before normalizing the condition, it is necessary to determine the underlying disease and eliminate it.
Moderate diffuse changes in bioelectrical activity can be reversed with timely diagnosis. They do not pose a terrible danger to human health and life. To do this, you need to undergo restorative treatment.
If such violations are left unattended, the consequences can be quite serious. With global lesions, motor skills are impaired, psychoemotional disorders occur, and children experience developmental delay.
The most serious dangers of pronounced changes in bioelectrical activity are considered to be seizures and epilepsy.
Main features
Dysfunction of the middle (deep) sections is often manifested by attacks of general weakness, a feeling of suffocation, dizziness, malaise, unmotivated fear, changes in pulse and blood pressure. These symptoms are similar to those of epilepsy and reflect the process of irritation of brain structures. Irritation of the cortical parts is more often manifested by behavioral deviations without pronounced neurological symptoms. Symptoms caused by the disorder depend on the location of the source of irritation:
- Frontal zone. Manifestations: motor dysfunction, twitching of the head and visual organs. When the adversive field is damaged, convulsions occur, often with confusion and loss of consciousness at the beginning of the attack.
- Temporal zone. Accompanied by auditory hallucinations. Damage to the opercular region initiates involuntary swallowing and chewing movements.
- Occipital zone. Manifestations: visual hallucinations, photopsia - the appearance of foreign objects in the field of view (dots, lightning, spots, lines).
- Parietal zone. It manifests itself as a sensitivity disorder - numbness, tingling, impaired perception of cold and hot objects, a change in the pain threshold. Damage to the central gyrus area is accompanied by epileptic seizures, which at the initial stage affect the muscles of the face and limbs.
- Cranial fossae. Manifestations: visual and auditory dysfunction, trigeminal neuralgia (affecting the trigeminal nerve), olfactory disorder.
Signs of cortical irritation with diffuse damage to multiple areas of the brain include convulsive syndrome. Convulsions develop according to the myoclonic type, regardless of the state (rest, movement) in which the patient is. Cortical myoclonus is characterized by a short-term, rapid course. At the same time, absence seizures—minor epileptic seizures—may occur while maintaining normal muscle tone. Grand mal epileptic seizures develop according to the following scheme:
- Aura. Headache, sleep disturbance, feeling unwell several hours or days before the attack.
- Phase of increased muscle tone. Loss of consciousness and balance. Synchronous, simultaneous contraction of muscles in the entire body. Duration – about 60 seconds.
- Clonus phase. Unsynchronous, chaotic contraction of body muscles. Duration – about 2 minutes.
After a seizure, the muscles relax and the patient falls into deep sleep. Upon awakening, the patient is often disoriented regarding space and time. He may have retrograde amnesia (cannot remember events preceding the attack). Signs of irritation in the area of diencephalic (deep) structures that make up the brain include epileptic seizures, deterioration of cognitive abilities, speech dysfunction, disorders of the autonomic nervous system, and psycho-emotional disorders.
Irritation in the area of the stem structures at the bottom of the cranium is accompanied by such disorders as confusion, disturbance of sleep and wakefulness, deterioration of memory and concentration. Irritation of the hypothalamic structures that make up the central parts of the brain is accompanied by the following symptoms:
- Malfunctions of the autonomic nervous system.
- Depressive state.
- Deterioration of attention and memory functions.
- Psychopathic disorders with symptoms characteristic of Korsakoff psychosis (retrograde amnesia, ataxia, disorientation, behavioral disorders).
Irritation in the area of the hypothalamic regions often initiates a deterioration in cognitive abilities, reversible speech dysfunction, and a change in personal perception of the position of parts of the torso and the entire body in space.
Signs
Directly depending on the location of the focus of irritation of the cerebral cortex, irritative symptoms will be obvious or hidden. Thus, when the second frontal gyrus or the posterior part of the middle gyrus is damaged, a person develops a tendency to convulsions - seizures with twitching of the eyes, head, and other parts of the body.
Whereas with irritation of the cerebral cortex in the area of the temporal lobe, auditory hallucinations are observed. And when a lesion forms on its inner part, there will be olfactory disruptions. Irritation of the opercular part leads to swallowing, as well as chewing and slurping uncontrolled movements.
When irritating the midline structures of the brain, there is a high risk of malfunctioning of the thalamic centers:
- cognitive impairment – understanding of spoken speech;
- distortion of a person’s perception of his own body;
- when there is a malfunction in the subthalamus of the hypothalamus, spatiotemporal disorientation appears;
- formation of endocrine and gynecological disorders.
Meanwhile, irritation of the diencephalic structures of the brain will be characterized by a disorder of subcortical formations - failures of thermoregulation, deterioration of sleep, nervous tics, or enuresis. With pathological excitation of the occipital part of the organ, memory lapses and visual hallucinations are observed - the patient sees flashes of light or lightning.
Apart from dysfunction of the median structures of the brain, the picture of the disorder in the appendage is so typical that a specialist can make a diagnosis already during the initial examination - excessive growth of the nose, tongue, or external genital organs, severe obesity.
If there is a malfunction in the area of the anterior/posterior cranial fossa, then the symptoms resemble those in the case of a stroke - the disorder is observed in the auditory, optic, facial nerve, with their paresthesia and paralysis.
Diagnostics
The main diagnostic method is a study in EEG format (electroencephalogram). During the study, bioelectric potentials of brain structures are recorded, which is reflected in certain patterns (waves, amplitude, rhythm). Irritation of brain areas manifests itself as:
- Desynchronization, uneven amplitude of the alpha rhythm.
- Increase in volume in the general structure of oscillations and amplitude of the beta rhythm.
- The appearance of a large number of sharp peaks in the overall wave pattern.
Signs revealed during EEG studies resemble epileptiform changes. To establish the primary causes of disorders, instrumental diagnostics are carried out, which makes it possible to identify the underlying disease. For this purpose, examinations are prescribed in the format of MRI, CT, ultrasound, angiography, positron emission tomography. Neuropsychological diagnostics are carried out to identify the nature and degree of disorders in the emotional, speech, and cognitive spheres.
Mental dysfunction due to damage to the diencephalic parts of the brain
The diencephalic regions of the brain are closely connected with the mediobasal regions of the frontal and temporal lobes of the brain.
Damage to these areas occurs during pathological processes that arise in formations located in the midline or affecting these formations (tumors of the pituitary gland, third ventricle, septum pellucidum, basal parts of the brain).
Neuropsychological disorders are often accompanied by autonomic disorders and hormonal disorders (especially with lesions at the pituitary level).
In the neuropsychological status of patients, there are disturbances in the sleep-wake cycle and a decrease in the general functional state.
There are changes in the emotional and personal sphere in the form of increased emotional reactivity, instability of emotional reactions (for example, the occurrence of tearfulness or, conversely, mild euphoria).
Mild personality disorders in the form of some uncriticality and inadequacy are also possible.
Unlike brainstem patients, this category of patients exhibits more severe memory impairments of a modality-nonspecific type, which are associated with increased inhibition of traces in the form of retroactive and proactive inhibition that arise under conditions of both homogeneous and heterogeneous interference.
Electrical stimulation of the thalamic nuclei and mesencephalic reticular formation usually causes simultaneous changes in short-term and long-term verbal and figurative memory, combined with changes in attention span.
Features of memory during point electrical stimulation of the median center of the thalamus were described by V.M. Smirnov.
He observed superoptimal states in which, along with general mental activation, the volume of short-term memory can almost double.
Smirnov pointed out that in terms of the number of zones, the point electrical stimulation of which caused changes in memory, the nuclei of the thalamus - the pulvinar and posterolateral - are in first place.
However, the effects of repeated electrical stimulation of these brain areas to influence short-term memory depended significantly on the general functional background.
Long-term studies of memory with electrical stimulation of the brain are reflected in the works of Ojemann. He showed that electrical stimulation of the thalamus pad can lead to erroneous naming of an object while maintaining expressive speech and forgetting the image presented immediately before stimulation.
Electrical stimulation of the ventrolateral nucleus of the thalamus in patients with parkinsonism during stereotactic operations was carried out against the background of the presentation of stimuli, interference (distraction), or at the time of a request to name an object presented on a slide.
It turned out that when stimulating the left-sided nuclei of the thalamus opticus, stimulation caused a decrease in the number of errors in the answer if it coincided with the task, and an increase if it coincided with the answer. Stimulation during distraction did not affect the correctness of the answer.
At the same time, it was noted that stimulation of the left thalamus causes a specific alertness reaction, which fixes attention on the presented verbal information.
Studies of long-term memory in patients after surgery have shown that stimulation of the left-sided nuclei of the thalamus affects not only short-term memory, but also long-term memory.
When stimulating the medial central zone of the left ventrolateral nucleus of the thalamus, the correct naming of objects was impaired, and the zone of the nucleus, the stimulation of which led to the deterioration of this type of long-term memory, was geographically smaller than the zone, the stimulation of which affected short-term memory.
Symptoms of thalamic damage are extremely complex and resemble dysfunction in various areas of the brain. S.B. Buklina emphasizes that in many patients with AVM of the thalamus, memory disorders were combined with disturbances in praxis, rhythm assessment, and optical-spatial functions.
On the one hand, this may be due to the fact that the thalamus has numerous connections with different areas of the brain.
On the other hand, with hemorrhage there is often concomitant destruction of the nearby internal capsule, connections with the subcortical nodes and other pathways.
Half of the patients studied had Korsakoff's syndrome, which is much more than with damage to the hippocampus! In several patients, the phenomenon of neglect was observed (left-sided or right-sided, depending on the profile of the patient’s lateral asymmetry).
After surgery, the most common neurological symptom was hemianopsia, often combined with hemiparesis and hemihypesthesia.
A number of patients exhibited pseudoathetosis, “thalamic brush,” tremor, and hyperpathy. After surgery for malformations of the left thalamus, peculiar speech disorders similar to cortical disorders came to the fore.
During operations on the right thalamus, predominantly emotional-volitional disorders and thinking disorders were noted.
The hypothalamus is a key structure for implementing the most ancient reinforcing function of emotions and for solving the universal behavioral task of maximizing and minimizing the emerging emotional state: approach or avoidance.
After all, it is the receipt of desirable, emotionally positive stimuli or the elimination of unwanted, emotionally negative ones, and not the satisfaction of any need, that serves as direct reinforcement during learning.
Thus, in rats it is impossible to develop an instrumental reflex when food is introduced through a cannula into the stomach (that is, bypassing taste buds), although such a reflex is developed when morphine is introduced into the stomach, which very quickly induces a positive emotional state in the animal.
The same morphine, due to its bitter taste, ceases to be a reinforcer if it is administered orally. Evidence of the involvement of the neocortex in emotional reactions has been obtained in animals using neurophysiological methods and in humans through clinical observations.
For example, it was found that a rage reaction easily occurs in decorticated animals as a result of a deficiency of inhibitory influences on the functions of the posterior hypothalamus.
It is noted that the clinical (including emotional) manifestations of the disease depend on a number of factors: location, nature, stage of the disease, age of the patient, etc.
In general, emotional and affective disorders that arise from lesions of the pituitary-diencephalic region of the brain occur, as a rule, in the form of a disorder of background states with greater preservation of criticism, i.e. personal attitude towards one’s emotional defect.
Researchers note that when the thalamus is damaged, there are not only diencephalic, but also hemispheric symptoms (speech defects in the case of left-sided localization, gnostic defects in the case of right-sided localization). There may be symptoms of dysfunction of the frontal lobes of the brain (lack of spontaneity, uncriticality, tendency to perseveration, etc.).
When the hypothalamic region is damaged, the so-called amnestic syndrome is often formed.
It has a modality-nonspecific nature and varying degrees of severity, varying in different patients from mild manifestations that can only be detected in special clinical and experimental conditions, to the scale of memory impairment characteristic of Korsakoff syndrome.
However, regardless of the depth of the mnestic defect, patients retain the orientation towards memorization and subsequent reproduction, as well as the ability to control the implementation of mnestic activity.
This fact allows us to say that memory loss with damage to the hypothalamic region is not associated with defects in voluntary regulation.
During the neuropsychological examination, one can see that the learning curve for 10 words corresponds to the so-called general organic type, when the memorization process is extended over time, fluctuates in the level of productivity and does not reach one hundred percent of the final result, being limited to a maximum of productivity at the level of 7–8 words.
In this case, the task of memorization is accepted by the patient, and its implementation is controlled by him. Reproduction of material immediately after its presentation is 5–6 words, which corresponds to the lower limit of the norm.
It is also possible to retain in memory for 2–3 minutes under conditions of an “empty” pause the material that has just been reproduced, which indicates the relative safety of the link in transferring information from short-term memory to long-term memory.
However, increasing the pause to 4 minutes or more, as a rule, leads to a decrease in playback productivity. N.K. Korsakov and L.I. Moskovichiute suggests that this phenomenon is based on the mechanism of disruption of the very function of trace formation at the stage of transferring traces to a long-term storage system.
The introduction of interference leads to the emergence of retroactive inhibition, since due to the implementation of the interfering task, the possibility of updating the traces of learning preceding the interference is blocked.
Removal of interfering influences can lead to the emergence of reminiscences, which is one of many experimental evidence of the inhibitory, and not destructive, effect of the interfering task in relation to the memory trace.
Memory impairments occur against the background of a decrease in the level of activation, which exhibits significant fluctuations.
Therefore, memory disorders are also fluctuating in nature, and the degree of their severity can fluctuate on different days, during one study, or even during the performance of one task.
The range of fluctuations is associated with the stage of development of the pathological process and its effect on lower-lying brain stem structures.
A decrease in the level of activation also manifests itself in the emotional sphere in the form of a general flattening of affective processes, their monotony, lethargy, and a narrowing of the field of emotionally significant stimuli.
In severe cases, disturbances of consciousness appear in the form of disorientation in place, time, and sometimes in the circumstances of one’s own life.
As a rule, these disturbances of consciousness pass without confabulations. The attention function is also deficient in these patients.
With a general decrease in both voluntary and involuntary attention, it, like memory impairment, has a fluctuating nature, is unstable and can rise to a higher level with external, additional stimulation.
Dysfunction of the hypothalamic-pituitary region is often associated with Itsenko-Cushing's disease.
Itsenko-Cushing's disease is a neuroendocrine disease characterized by increased production of adrenal hormones, which is caused by excessive secretion of adrenocorticotropic hormone (ACTH) by cells of hyperplastic or tumor tissue of the pituitary gland (in 90% the cause of this disorder is microadenoma).
As a result, hyperproduction of cortisol (hypercortisolism), corticosterone, aldosterone and androgens occurs by the adrenal cortex.
Researchers emphasize the connection between hormonal dysfunction that occurs with pituitary adenoma and cognitive impairment.
The fact is that there is a relatively high concentration of cortisol receptors in the prefrontal cortex, amygdala and hippocampus, and cortisol can affect memory performance.
Chronic hypercortisolism has a detrimental effect on the ability to remember new information. However, a sharp rise in cortisol levels can increase the reproduction of emotionally charged stimuli compared to neutral ones.
It has been suggested that high levels of cortisol require the simultaneous presence of norepinephrine in the amygdala in order for the amount of information to be remembered to increase.
At the same time, such studies are often criticized due to failure to comply with all the necessary conditions for selecting patients to participate in the experiment.
Thus, not all studies measure hormone levels on the day of testing, and often do not distinguish between men and women, or between young and elderly patients, despite the fact that these factors are very important in cases where the influence of sex hormones is studied.
In addition, patients with hormone-producing tumors often find themselves in the same experimental group with hormone-non-producing tumors, which also complicates the interpretation of the results.
Finally, the very nature of the connection between the pituitary and adrenal hormones does not always make it possible to determine which hormone affects the deterioration of memory, attention and other cognitive functions.
Treatment options
Treatment of the pathological condition, which is manifested by general cerebral changes of an irritative nature, is aimed at eliminating its causes. Treatment is carried out for the primary disease that provoked the corresponding symptoms. In case of infection, antibacterial and antiviral drugs are prescribed. Other medicines:
- Nootropic, stimulating cellular metabolism in nervous tissue, protecting neurons from damage.
- Regulating cerebral blood flow, improving the rheological properties of blood.
- Antidepressants, sedatives.
The therapy program involves taking medications that strengthen the vascular wall, regulate cholesterol levels and lipid metabolism, and prevent the formation of blood clots. The patient should avoid head injuries and excessive physical and mental stress. Therapeutic measures include neurocorrection - procedures during which brain functions are redistributed and compensatory mechanisms are activated.
Irritation (irritation) of brain structures leads to behavioral disorders and neurological symptoms, which deteriorates the patient’s quality of life. The pathological condition is a consequence of a primary disease, which is identified by a doctor during a diagnostic examination and is treated first.
652