Prosopalgia is a collective clinical concept that combines all pain syndromes that occur in the facial area. The complex anatomical and functional organization of the facial structures and nervous system of this area determines the diversity of pathogenetic mechanisms of pain.
Among the latter, we can distinguish compression, inflammatory, and reflex. The great individual significance of the face and increased attention to this part of the human body determines the frequent occurrence of prosopalgia of psychogenic origin. The neurotic component is often layered on top of any pathological processes in the facial area, which should certainly be taken into account in the treatment of facial pain of various natures. Due to its variable etiology, prosopalgia is the subject of supervision of doctors of various clinical specializations - neurology, otolaryngology, ophthalmology, dentistry, psychiatry.
Some information about the disease
Due to the fact that the facial part has a complex anatomical organization, pain in this area can appear for various reasons. It will be a little difficult to define. There may be damage to the facial or dental nerve or something else. In any case, only a specialist with examinations and tests can answer the question of why left-sided prosopalgia formed. Treatment of this disease is very difficult and long-term. As a rule, patients with this diagnosis turn to such specialists as an otolaryngologist, a neurologist and a therapist.
Left-sided prosopalgia: causes of the disease
This disease appears due to a number of factors, of which there are a large number.
When the jaw and teeth are damaged, odontogenic pain occurs. Unpleasant sensations are transferred to the face. The causes of this disease are most often caries, damage to the pulp or dental nerve. In the presence of such symptoms, the pain is pulsating in the jaw area. If you drink cold water or hot tea, the discomfort becomes stronger. To diagnose and treat left-sided facial prosopalgia, you will need to consult a dentist.
Another common type of this disease is Slader syndrome. With it, pain occurs in the area of the eyes, tongue and ears. Moreover, these unpleasant sensations can radiate to the neck and shoulder blades.
Carotidynia is characterized by pain in the face due to inflammation of the carotid arteries. With such left-sided prosopalgia, unpleasant sensations occur in the area of the neck and teeth. Typically, a person suffers from this disease for several hours. It becomes especially unpleasant at the moment when someone touches the carotid arteries.
Reasons why prosopalgia occurs
Facial pain can come from many anatomical structures. At the same time, the symptom also indicates inflammation of the nerves of the face. Understanding what is causing the condition is the main task of the doctor prescribing treatment for facial pain.
Neurogenic prosopalgia
- Frey's syndrome. This syndrome characterizes inflammation of the mandibular nerve. The cause of the disease is pathology of the parotid gland: mumps, sialadenitis, abscess, postoperative disorders. For treatment, it is necessary to identify the pathology of the salivary gland and eliminate it, and then deal with the inflammation of the mandibular nerve.
- Sluder syndrome is an inflammation of the nuclei of the pterygopalatine nerve plexus. The pain spreads throughout the face: in the area of the upper and lower jaw, nose, eyes, TMJ. It can also radiate to the back of the head and neck.
- Trigeminal neuralgia is characterized by excruciating pain in various areas of the face. Pain syndrome occurs with any skin irritation: applying makeup, washing, shaving, etc.
- Postherpetic neuralgia develops after suffering from herpes. Herpetic rashes are localized along the nerve tracts. After regression of the pathology, neuralgia often appears, which is difficult to treat.
Myofascial prosopalgia
Myofascial prosopalgia is similar to trigeminal neuralgia, but in this case it is associated with muscle pathology. Redistribution of the load on the TMJ, stress, involuntary contraction of the facial muscles, TMJ injuries - all this is the cause of myofascial pain. The pathology can imitate ear inflammation, diseases of the salivary glands, arthrosis and arthritis of the TMJ. Her treatment is based on stress relief, bite correction, examination and treatment of the temporomandibular joint.
Otalgia
Pain in the ear area, spreading to the entire face, can be caused by inflammatory diseases, vascular pathology, venous sinus thrombosis, or damage to the third cervical vertebra. The cause of otalgia can also be dysfunction of the TMJ.
TMJ dysfunction
With dysfunction of the temporomandibular joint, pain is localized not only in front of the auricle, but also on the face (forehead, cheeks, temples, lower and upper jaw). In addition to facial pain, dysfunction is accompanied by impaired joint mobility, pain when chewing, and articulation. Chronic TMJ dysfunction requires surgical treatment. Arthroscopy surgery is widely used (helps in 90% of cases).
Atypical prosopalgia
Atypical prosopalgia characterizes facial pain, the organic cause of which could not be identified. This is a diagnosis of exclusion. Pain sensations can be either unilateral or bilateral, spreading to the neck and back of the head. The symptom mainly occurs during the daytime, during stress and emotional overload. Facial pain may not bother you for several months, after which it appears again.
Atypical prosopalgia can imitate toothache, inflammation of the TMJ, and pathologies of the salivary gland. However, treatment of these diseases does not lead to improvement in the patient's condition.
What is Charlen syndrome?
With this disease, the main pain is localized in the nose and inner corners of the eye. On top of everything else, conjunctivitis and runny nose are added to it. Unpleasant sensations also occur in the face, temples and forehead. In this case, joint movements are limited, a peculiar crunch appears, and chewing functions are disrupted when eating any food.
When the trigeminal nerve is damaged, very strong unpleasant sensations are observed in the facial area. When taking antispasmodic or analgesic medications, the pain does not disappear. Immediate assistance from a specialist is required.
Other reasons for the development of left-sided facial prosopalgia are migraine or otitis media.
Trigeminal neuralgia - Fothergill's disease
With this disease, the main pain is localized in the nose and inner corners of the eye. On top of everything else, conjunctivitis and runny nose are added to it. Unpleasant sensations also occur in the face, temples and forehead. In this case, joint movements are limited, a peculiar crunch appears, and chewing functions are disrupted when eating any food.
When the trigeminal nerve is damaged, very strong unpleasant sensations are observed in the facial area. When taking antispasmodic or analgesic medications, the pain does not disappear. Immediate assistance from a specialist is required.
Other reasons for the development of left-sided facial prosopalgia are migraine or otitis media.
According to Ksenia Dyachenko, with this disease, pain occurs in the form of an acute attack, concentrated near the eyes and ears, in the dentofacial area, tongue and palate; can radiate to the neck, shoulder and shoulder blade area. Painful sensations are often accompanied by vegetative symptoms: patients complain of a stuffy nose, involuntary lacrimation, and swelling of the face.
This rather rare disease is characterized by paroxysmal facial pain, covering the inner corner of the eye and the root of the nose on one side of the face. Where the exits of the external nasal and infraorbital nerves are located, local areas of severe pain are noted. With Charlen's syndrome, injection of the conjunctiva of the eyeball, a “stuffy nose,” and spasmodic closing of the eyelids (blepharospasm) are also observed.
A rare syndrome in which sharp, paroxysmal shooting pain occurs in the oral cavity, tonsils, and root of the tongue with any strain: speaking and coughing, chewing, yawning, swallowing (especially cold drinks). The pain may radiate to the ears or neck area; with the otalgic form of neuralgia, the face hurts exclusively in the ear area.
The slightest mechanical impact on the tissues of the soft palate, tonsils, or pressure on the protrusion near the base of the ear (tragus) can cause an attack. The painful attack does not last long, from seconds to several minutes, but is accompanied by extremely dangerous symptoms: a sharp drop in blood pressure, slow heart rate, even fainting. The latter is typical if the cause of neuralgia is a tumor of the pharynx.
This type of neuralgia causes paroxysmal pain in the angles of the lower jaw, as well as in the larynx - on one or both sides, concentrated in the area of the apex of the thyroid cartilage or at the level of the bone to which the root of the tongue (hyoid) is adjacent. The pain syndrome spreads upward (to the eyes and ears) and downward (to the chest), accompanied by increased salivation, coughing, and bouts of hiccups. Pain occurs when swallowing, yawning or coughing, trying to blow your nose, or simply when suddenly moving your head.
What is otalgia?
This phenomenon characterizes itself as ear pain. Unpleasant sensations are localized not only here, but also in parts of the face. A fairly large number of diseases can have such symptoms. You should consult a specialist and undergo an examination. Possible nasopharyngeal tumor or venous sinus thrombosis. Also, one should not exclude the possibility that it is most likely just a migraine. One of the possible diseases with this symptomatology is idiopathic otalgia. It is characterized by the fact that ear pain occurs due to unknown reasons.
There is also red ear syndrome. With this disease, the discomfort is very painful and radiates to the jaw and back of the head. The blood vessels dilate and the skin takes on a reddish tint. And the temperature in the auricle becomes significantly higher.
Otalgia
This phenomenon characterizes itself as ear pain. Unpleasant sensations are localized not only here, but also in parts of the face. A fairly large number of diseases can have such symptoms. You should consult a specialist and undergo an examination. Possible nasopharyngeal tumor or venous sinus thrombosis.
There is also red ear syndrome. With this disease, the discomfort is very painful and radiates to the jaw and back of the head. The blood vessels dilate and the skin takes on a reddish tint. And the temperature in the auricle becomes significantly higher.
Facial pain concentrated in one or both ears can cause dozens of diseases, including: nasopharyngeal tumor; vertebral artery aneurysm; venous sinus thrombosis; migraines or cluster headaches; Idiopathic otalgia is also common, in which pain in the ear occurs for unknown reasons.
Red ear syndrome, or erythrootalgia, is also known. This disease is characterized by severe burning pain in the ear itself, spreading to the lower jaw, forehead and back of the head. Due to the expansion of blood vessels, redness of the skin occurs, and the temperature in the auricle locally increases.
Facial pain in the ear area is characteristic of many diseases, including:
- neoplasms of the nasopharynx;
- vertebral artery aneurysm;
- migraines and cluster headaches;
- inflammation of the glossopharyngeal nerve.
In addition, there is idiopathic otalgia, the origin of which has not been established.
Characteristics of atypical prosopalgia
This disease is also characterized by pain in the face and neck. Only the reason for their occurrence is not entirely clear and known. The disease usually develops in women in old age. This usually includes pain of a vegetative-vascular nature. In the case when the patient suffers from atypical prosopalgia, unpleasant sensations always follow him in the face and move to the neck. The pain affects one side. If it is bilateral, then it is characterized by asymmetry.
This disease also includes glossalgia, in which pain is observed in the tongue area. At the moment of an emotional outburst during the day, unpleasant sensations increase or, conversely, decrease. As a rule, it is very difficult for patients to describe the nature of the pain.
Medical Scientific and Practical Center for Vertebrology and Neuroorthopedics, Professor M.L. Kurganov
Prosopalgia is a collective clinical concept that combines all pain syndromes that occur in the facial area. The complex anatomical and functional organization of the facial structures and nervous system of this area determines the diversity of pathogenetic mechanisms of pain.
Among the latter, we can distinguish compression, inflammatory, and reflex. The great individual significance of the face and increased attention to this part of the human body determines the frequent occurrence of prosopalgia of psychogenic origin. The neurotic component is often layered on top of any pathological processes in the facial area, which should certainly be taken into account in the treatment of facial pain of various natures. Due to its variable etiology, prosopalgia is the subject of supervision of doctors of various clinical specializations - neurology, otolaryngology, ophthalmology, dentistry, psychiatry.
Causes of prosopalgia
An inflammatory reaction can act as an etiofactor of facial pain. Most often, prosopalgia of inflammatory origin occurs with sinusitis. It can be observed in otitis media, ophthalmological diseases (iridocyclitis, uveitis, conjunctivitis, keratitis, corneal ulcer), TMJ arthritis, and have an odontogenic etiology (pulpitis, periodontitis). Prosopalgia can occur with inflammatory lesions of the vessels of the facial area, for example, with Horton's disease. Often, neurogenic prosopalgia has an inflammatory etiology with neuralgia of the glossopharyngeal nerve, trigeminal neuralgia, Oppenheim syndrome, pterygopalatine ganglionitis, geniculate ganglionitis.
On the other hand, neurogenic prosopalgia may have a compression genesis, i.e., arise as a result of compression of nerve trunks or nodes due to changes in the relative position of the anatomical structures of the facial area, narrowing of bone and intermuscular nerve canals, development of tumor formations, etc. Compression etiology may have vascular prosopalgia, for example, carotidynia due to compression of the carotid artery.
The reflex mechanism of pain syndrome is often realized in odontogenic and neurogenic facial pain. The cause of prosopalgia in such cases is pathological reflex impulses coming from chronic infectious foci. An example is neuralgia of the ear ganglion. Myogenic prosopalgia of reflex genesis occurs with myofascial syndromes in the neck and shoulder girdle. Other causes of myogenic prosopalgia may include TMJ dysfunction (Costen syndrome), bruxism, and myofascial syndrome in the masticatory muscles.
Prosopalgia of psychogenic origin often occurs in suspicious, emotionally labile people against the background of overwork, chronic psycho-emotional discomfort, or as a result of an acute stressful situation. Often, psychogenic prosopalgia is observed in persons with hysterical neurosis, neurasthenia, and depressive neurosis. It can occur as part of psychiatric diseases such as schizophrenia, psychopathy, manic-depressive psychosis.
In some cases, prosopalgia is iatrogenic. Thus, Oppenheim syndrome can occur after ophthalmological operations; tooth extraction and other dental interventions can trigger the development of dental plexalgia or atypical odontalgia. One of the causes of neurogenic facial pain is damage to nerve structures during operations in the facial area. In addition, a number of facial pains do not have a clearly established etiology. For example, cluster headache, atypical prosopalgia, chronic paroxysmal hemicrania.
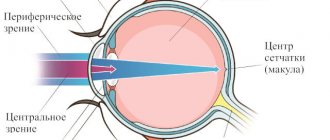
Classification of prosopalgia
Facial pain is classified primarily by mechanism of development. There are vascular, neurogenic, myogenic, psychogenic, symptomatic, atypical prosopalgia and painful ophthalmoplegia. Vascular facial pain includes fascicular cephalgia, paroxysmal hemicrania, Horton's disease, idiopathic sudden cephalgia (ISH), SUNCT syndrome. Neurogenic prosopalgia includes neuralgia of the trigeminal and glossopharyngeal nerves, ganglionitis and ganglioneuritis of the nerve ganglia of the facial region. Depending on the etiology, symptomatic prosopalgia is divided into ophthalmogenic, odontogenic, otorhinogenic, and viscerogenic. Atypical includes pain that does not fit into the clinical picture of any of the types of prosopalgia indicated in the classification. They are often caused by a combination of several pathogenetic mechanisms and have a psychogenic component.
Clinical features of prosopalgia
Facial pain of various origins differs in its clinical features regarding the nature, duration, paroxysmalness, and vegetative coloring of the pain syndrome. These distinctive features, as well as accompanying symptoms (if any), enable the neurologist to determine the type of prosopalgia, which is fundamental in the diagnosis and subsequent treatment of facial pain.
The permanent (constant) type of pain syndrome is more typical for myogenic, psychogenic and symptomatic prosopalgia. It may occur with episodes of increasing and decreasing pain. Paroxysmal pain phenomenon with intense painful attacks of variable duration against the background of complete or almost complete absence of pain in the interictal period is typical for neurogenic and vascular prosopalgia. A distinctive feature of the latter is the presence of a pronounced vegetative component - during paroxysm, swelling, lacrimation, hyperemia of the skin area, rhinorrhea, nasal congestion, redness of the conjunctiva, etc. are observed. Symptomatic, myogenic and psychogenic prosopalgia, as a rule, is bilateral in nature. Moreover, the latter may be distinguished by the asymmetry of the pain phenomenon in the halves of the face. Vascular, neurogenic and atypical facial pain is usually unilateral.
Irradiation of pain is more typical with neurogenic and vascular prosopalgia, but can also be observed with facial pain of symptomatic origin. In addition, symptomatic prosopalgia is often reflexive in nature. The most illustrative example is odontogenic prosopalgia, caused by the occurrence of pain in the Zakharyin-Ged zones: mandibular, nasolabial, maxillary, frontonasal, temporal, sublingual, mental, laryngeal. Each zone is a reflection of the pathology of certain teeth, while toothache may be absent.
Diagnosis of prosopalgia
In most cases, facial pain in itself is not a diagnosis, but rather a syndrome. In this regard, it is important to identify/exclude the underlying disease that caused prosopalgia. During diagnosis, a neurologist-algologist carefully studies the various characteristics of the pain phenomenon, palpates the facial muscles, and identifies trigger points (places of intense palpation pain). The exclusion/confirmation of the symptomatic nature of facial pain is carried out with the participation of an ophthalmologist, dentist, and otolaryngologist.
If necessary, dental radiography, orthopantomogram, radiography of the paranasal sinuses and temporomandibular joint, otoscopy and pharyngoscopy, measurement of intraocular pressure, examination of eye structures, etc. are performed. In order to identify inflammatory changes, a clinical blood test is prescribed. Psychogenic and atypical prosopalgia are an indication for consultation with a psychiatrist or psychotherapist with psychological testing and pathopsychological examination.
Treatment of prosopalgia
Treatment of facial pain depends entirely on its etiology. Symptomatic prosopalgia first of all requires treatment of the underlying disease - otitis media, sinusitis, pulpitis, etc. With inflammatory genesis, neurogenic, vascular and myogenic prosopalgia are treated by prescribing anti-inflammatory medications (diclofenac, indomethacin, ibuprofen, nimesulide, etc.). To relieve pain at trigger points, therapeutic blockades with the administration of corticosteroids and local anesthetics can be performed. For trigeminal neuralgia, the use of carbamazepine is effective, for ganglionitis - ganglion blockers (benzohexonium, pentamine), for Horton's disease - corticosteroids (prednisolone). Physiotherapeutic methods are additionally used for anti-inflammatory purposes: hydrocortisone ultraphonophoresis, DDT, magnetic therapy, electrophoresis.
Therapy for facial pain of compression origin, in addition to anti-inflammatory treatment, includes vascular (nicotinic acid, aminophylline) and decongestants (antihistamines, diuretics) and vitamins. B. Failure of conservative therapy is an indication for surgical treatment (for example, microsurgical decompression of the trigeminal nerve). Persistent prosopalgia in ganglioneuritis is an indication for removal of the affected ganglion; in trigeminal neuralgia, in such cases, a measure of temporary pain relief is radiofrequency destruction of the trigeminal nerve root.
In many cases, a mandatory component of the treatment of facial pain is sedative therapy: soothing herbal preparations, mild tranquilizers (mebicar), antidepressants (St. John's wort extract, fluvoxamine, sertraline). If necessary, vegetotropic agents are prescribed (belladonna alkaloids + phenobarbital, belladonna extract). Therapy for psychogenic prosopalgia is carried out using psychotherapy methods and psychotropic drugs selected in accordance with the clinical characteristics: tranquilizers, neuroleptics, antidepressants. Electrosleep and darsonvalization are indicated.
What are the classifications of pain syndromes?
According to the mechanism of development, somatogenic, psychogenic, vegetative and neurogenic unpleasant sensations are distinguished. The first type is associated with the impact on the human body of damaging factors during injury. For example, pain when internal organs are damaged. Neurogenic syndrome appears due to damage to the structures of the central nervous system.
Vegetalgia occurs with pathologies of internal organs. Psychogenic pain refers to those unpleasant sensations that usually occur after strong emotional experiences or depression. In this case, the patient relies on his condition and describes the situation as he sees it at the moment.
Myofascial pain syndrome of the face
With dysfunction of the temporomandibular joint (also called Costen's syndrome), patients experience pain in the face not only in the place where the joint itself is located (slightly in front of the ear), but also in other areas - in the cheek, lower jaw, temple or forehead. At the same time, the joint is limited in movement and characteristically “clicks.”
Pain can be caused by problems with the non-inflammatory muscles of mastication (MFM), malocclusion, and various joint diseases. During the examination, the presence of local painful areas, a distinct crunch when the patient opens the mouth, limited movement of the lower jaw and displacement of the articular surfaces are observed.
It is based on overstrain of the muscles responsible for chewing and facial expressions, and the neck muscles with the formation of spasmodic areas (trigger zones) in them.
Myofascial pain syndrome is often misdiagnosed, mistaking its symptoms for manifestations of trigeminal neuralgia.
Causes of pathology
- Incorrect closure of the dentition at one or more points. The result of the different heights at which the teeth touch is disruption of the joint of the lower jaw. This can cause pain and spasms in the masticatory muscles and injuries to the maxillofacial apparatus.
- Stress, physical and mental fatigue. Some people hold back negative emotions and, during experiences, only grit their teeth in the literal sense of the word. Over time, tension in the facial and chewing muscles becomes a habit and leads to the formation of myofascial syndrome.
- Depression. A chronic depressed state leads to disruption of the brain mediators that are responsible for normal muscle tone.
- Osteochondrosis of the cervical spine. The disease causes overstrain of the masticatory muscles of a reflex nature.
- Jaw fractures and other injuries to the temporomandibular joint.
Left-sided prosopalgia: symptoms of the disease
One of the most distinctive signs of this disease is very strong pain in the facial area. They can be different in character. Some people have paroxysmal or aching discomfort, while another patient has acute ones. It all depends on the cause of left-sided prosopalgia. It also happens that the pain increases when swallowing chewed food or pressing on the jaw or teeth.
In addition to unpleasant sensations in the facial area, other symptoms appear that also relate to this disease:
- severe increase in body temperature;
- lack of desire to eat;
- nasal congestion;
- an increase in the size of the lymph nodes;
- disturbance of restful sleep due to severe pain;
- redness of the skin and the appearance of a rash on it;
- typical facial asymmetry;
- periodic tinnitus;
- fatigue and weakness;
- increased lacrimation;
- the appearance of a nervous tic.
Features of the disease
Dysfunctional facial pain is characterized in a special way:
- the main risk group is women over 45 years of age;
- absence of trigger points, trigger zones, autonomic disorders;
- the localization of pain does not coincide with the innervation of the anatomical zone;
- unpleasant sensations appear almost every day;
- pain appears in one half of the face, its character is aching, dull, debilitating;
- the patient is fixated on pain and is often emotionally unstable;
- an attack of pain is often provoked by temperature changes, stress, or dental intervention.
The disease lasts for many years, becoming chronic and alternating between remissions and subsequent exacerbations.
Pain in the facial area can be caused by a disease of the nervous, vascular, muscular, dental systems or diseases of the ENT organs, eyes, skin, or can occur spontaneously. This severe pain syndrome is called atypical facial pain. Most often, the cause of its appearance is neuropsychic disorders caused by constant depression, stress, severe anxiety and increased excitability.
Facial pain may be accompanied by:
- asymmetry and swelling of the face;
- numbness of the face;
- swelling and nasal congestion;
- muscle spasms;
- loss of smell and taste;
- blurred vision;
- “noise” in the ears;
- nervous tics;
- severe dryness or excessive discharge from the nose or eyes;
- redness and itching of the skin.
Typical facial pain can be caused by injury, post-traumatic stress disorder, severe headache (migraine), inflammation, dysfunction or malfunction of any system or organ. Most often, severe facial pain is caused by inflammation of a nerve or nerve plexus - neuralgia (neuralgia of the trigeminal, glossopharyngeal, superior pharyngeal nerve or pterygopalatine nerve ganglion), as well as dental diseases (pulpitis, deep caries, osteomyelitis, abscess, etc.). Facial pain can occur with various diseases of the ENT organs - sinusitis, sinusitis.
In addition, severe facial pain can be caused by severe pathologies of the cardiovascular system: hypertensive crisis, myocardial infarction or stroke.
According to the nature of the pain, facial pain can be:
- migrating or concentrated in one place;
- pulsating or spasmodic;
- dull, aching or sharp.
The pain may be concentrated in the face or spread to the entire head or other parts of the body.
If severe facial pain occurs, it is strictly forbidden to self-medicate and uncontrollably take painkillers or other medications. This approach can lead to serious and life-threatening consequences for the patient. Only a doctor, after a comprehensive examination of the patient and analysis of the symptoms of the disease, can select an effective and safe treatment regimen.
How is the disease diagnosed?
This process is very long. It includes several stages. To begin with, the specialist collects all the information and analyzes the person’s diseases. After this, the doctor asks about what worries the patient and finds out the causes of the listed symptoms. If necessary, the therapist then gives a referral to such specialized specialists as an otolaryngologist, a neurologist and a dentist. It should be noted that this procedure is not always mandatory.
Then you will need to undergo an x-ray examination. Thanks to him, it will be possible to find out the nature of the unpleasant sensations.
A general blood test is also a mandatory procedure. From its results we can tell whether there is inflammation or not.
Magnetic resonance imaging is prescribed if, in case of left-sided prosopalgia, diagnosis using previous methods did not give a final conclusion on the disease. Using this procedure, the source of inflammation is established, and, accordingly, you can find out the cause of the development of the disease.
They also test for the presence of inflammatory processes on the mucous membrane. Note that these methods are used only if the others did not help.
In addition to the procedures described above, the therapist and specialists can refer you to other diagnostic procedures. In this case, it is necessary to strictly adhere to the prescribed therapy and take only those medications prescribed by the doctor. You should not self-medicate. This will only make the situation worse. Remember that timely access to a medical facility guarantees recovery without complications.
How is the treatment carried out?
There is no single list of interventions for this disease. For left-sided prosopalgia, treatment depends on the causes of its occurrence. In addition, the specialist focuses on the nature of the unpleasant sensations and the reasons for their development.
Usually, first of all, the doctor tries to help the patient get rid of pain with an injection in the part of the face where it arose. Why injections, can't you just get by with pills? Unfortunately, in this case, such medications do not help at all.
What procedures does a specialist prescribe for a disease?
Sometimes the patient is sent to the physical room. Here the patient undergoes physiotherapeutic procedures, where painkillers are used. For example, for left-sided prosopalgia, a disease of the nervous system, electrophoresis with novocaine is often prescribed. Treatment methods such as hydrocarbon treatment, magnetic therapy and laser therapy are also carried out. If there is inflammation in the human body and the process develops, then it is treated with antibiotics and anti-inflammatory drugs.
A general recommendation for all patients is to take vitamins. This is what will increase the body’s resistance to all kinds of harmful bacteria, and also improve immune protection.
What is the prevention of prosopalgia?
In order for you to get sick less, you should pay more attention to your health and lifestyle. Namely, as mentioned above, strengthen the immune system and the body’s protective function with the help of vitamins and hardening procedures. Everyone needs to avoid hypothermia. Because this can cause not only left-sided prosopalgia, but also upper respiratory tract infections. If you have diseases of the ears or teeth, you should immediately contact a specialist to avoid complications.
Of course, when the first symptoms of prosopalgia appear, you should go to the doctor and receive appropriate treatment. The sooner you take action, the easier and faster the disease will pass.