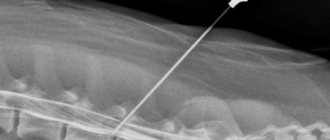
The procedure during which a special needle is inserted into the subarachnoid space is called a lumbar puncture (spinal, lumbar or spinal puncture, lumbar puncture or spinal puncture). The main purpose of the procedure is to collect cerebrospinal fluid (CSF) for further research, which will identify the exact causes of nervous diseases, infections and systemic pathologies. Lumbar puncture is also performed for therapeutic purposes. Before carrying out the procedure, it will be useful to know in what cases it is indicated and when it is prohibited. And when studying the technique of performing a lumbar puncture, the patient will understand that the manipulation is not dangerous to health. However, there is a possibility of some complications after it.
Basic information
Spinal cord puncture is a therapeutic and diagnostic procedure during which cerebrospinal fluid is extracted from the subarachnoid space through a special needle.
There is an opinion that lumbar puncture is dangerous, since during it the spinal cord can be damaged. To understand that this is not so, you need to delve a little deeper into embryology.
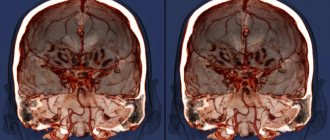
During fetal development, the central nervous system, which consists of the brain and spinal cord, develops from the fetal neural tube. All components of the nervous system (neurons, peripheral nerves, subarachnoid cisterns, cerebrospinal fluid, etc.) have the same origin. Therefore, by the composition of cerebrospinal fluid from the caudal region of the back, the condition of the entire nervous system can be assessed.
The spinal cord ends at the level of the 2nd lumbar vertebra
During fetal development, vertebrae grow faster than nerve tissue. For this reason, the spinal cord ends at the level of the 2nd lumbar vertebra with the conus medullaris. Further, thin threads extend to the junction with the sacrum.
Thanks to this structure, it is safe to puncture the spinal canal in this place. According to doctors, the phrase “spinal cord puncture” is incorrect, since there is no spinal cord at the puncture site, only its membranes and cerebrospinal fluid are located here.
Reference. The volume of cerebrospinal fluid in an adult is approximately 120 ml. It is updated after 5 days.
Not all people understand why they take a spinal cord puncture. Lumbar puncture is done to achieve the following goals:
- Study of biological material in laboratory conditions for glucose, certain cells, proteins and other components.
- Determination of cerebrospinal fluid pressure.
- Removing excess cerebrospinal fluid.
- Introduction of drugs into the nervous system.
Now you know why a cerebrospinal fluid puncture is taken.
No ads 1
How is the procedure performed?
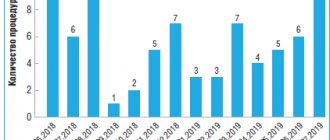
At the International Clinic Medica24, lumbar puncture is performed by doctors with extensive experience and high qualifications, which virtually eliminates any complications.
The procedure is carried out in full accordance with protocols accepted in world practice (Europe, USA, Israel). The obtained research data is entered into the medical history and will be accepted and unambiguously interpreted in any clinic in the world.
Medical supervision is required for some time after the procedure. The most comfortable conditions have been created in the hospital wards of our clinic, and professional medical staff provide the best standards of medical care.
A lumbar puncture is performed with a very thin needle, so the procedure itself is almost painless. However, local anesthesia is used during this procedure.
The needle is inserted into the space between the 3rd and 4th lumbar vertebrae (L3-L4) or between the 2nd and 3rd vertebrae (L2-L3).
During a lumbar puncture, the patient lies on his side in the fetal position - with his head down and his legs pressed to his torso.
A needle with a mandrel is used for the procedure. When the ligament and dura mater are pierced, resistance is felt. When the needle penetrates the subarachnoid space, its entry becomes easy (it seems to fall through). For an experienced doctor, this eliminates error, so additional means of visualization and control (ultrasound, CT) are not required for the procedure.
After the needle enters the subarachnoid space, a manometer is attached to it, and the cerebrospinal fluid pressure is measured.
The volume of cerebrospinal fluid collection is usually 10–20 ml. The total volume of cerebrospinal fluid is about 120 ml, and its daily secretion is 500 ml.
This means that cerebrospinal fluid is renewed four times during the day. Therefore, the collection of cerebrospinal fluid during lumbar puncture has virtually no effect on its volume, pressure and circulation.
Depending on the indications, a sample of cerebrospinal fluid is placed in one tube or divided into several tubes.
A sample is placed in one tube for biochemical analysis, measuring glucose and protein levels.
A sample of the liquid is placed in another tube to study its cellular composition.
The third - for bacteriological research.
The procedure takes very little time and can be performed in a day hospital at the International Clinic Medica24.
Indications for the procedure
As mentioned, a spinal tap may be performed for diagnosis or treatment. In the first case, the procedure is carried out when it is necessary to study the composition of the cerebrospinal fluid, identify pathogens in it, measure the pressure of the cerebrospinal fluid, as well as the patency of the subarachnoid (subarachnoid) space.
In the second case, the manipulation is carried out to evacuate excess cerebrospinal fluid and introduce medications (antibiotics or chemotherapy drugs) into the spinal canal.
Indications for lumbar puncture are divided into absolute and relative. In the first case, the procedure is mandatory, and in the second, it is recommended, but the decision is made by the doctor.
Lumbar puncture must be performed in the following cases:
- Infections affecting the central nervous system, for example, meningitis, encephalitis.
- Oncological formations in the membranes or structures of the spinal cord.
- Diagnosis of liquorrhea (leakage of cerebrospinal fluid) using radiocontrast agents.
- Subarachnoid hemorrhage (bleeding under the arachnoid membrane).
Relative indications include:
- Multiple sclerosis and other pathologies in which the myelin sheath of neurons is destroyed.
- Diseases characterized by systemic damage to peripheral nerves.
- Septic vascular embolism.
- Lupus erythematosus and other systemic connective tissue pathologies.
Meningitis is often preceded by an infection, and a lumbar puncture is performed to determine its cause.
During a lumbar puncture, the presence of pathogenic bacteria in the cerebrospinal fluid can be determined.
It is necessary to take cerebrospinal fluid for examination to determine intracranial pressure, the number of neutrophil granulocytes, and the presence of pathogenic bacteria (Haemophilus influenzae, meningococcus, pneumococcus).
A lumbar puncture is done to distinguish a stroke from other pathologies and to determine the cause of its development. A spinal puncture helps determine antibodies in the cerebrospinal fluid, then doctors talk about multiple sclerosis. If tuberculosis is suspected, the cerebrospinal fluid is examined for sugar, neutrophils and lymphocytes. A spinal tap is performed to detect syphilis in asymptomatic cases.
Reference. By measuring cerebrospinal fluid pressure, hydrocephalus (water on the brain) can be detected. When evacuating 50–60 ml of fluid, most patients feel relief.
Lumbar puncture in newborns is performed if meningitis is suspected. The study will help identify the causative agent of infection (viruses or bacteria). The study will also help to identify the level of protein and red blood cells in a child, because their deficiency increases the risk of infectious diseases.
No ads 2
Indications and contraindications
Lumbar puncture is necessary in the following cases:
- if you suspect infectious diseases of the central nervous system (encephalitis or meningitis);
- in case of suspected subarachnoid or intracerebral hemorrhage, if computed tomography cannot be performed or the study gives negative results;
- patients with high intracranial pressure due to hypertensive hydrocephalus, subarachnoid hemorrhage or benign intracranial hypertension;
- for administering medications into the spinal canal (antibiotics for meningitis).
A lumbar puncture of the spine is performed to exclude or confirm the diagnosis of neuroleukemia.
Contraindications to performing a lumbar puncture are infectious skin diseases at the site of the intended puncture, suspicion of the presence of a brain space-occupying lesion (abscess, tumor, subdural hematoma), especially in the posterior cranial fossa, and a marked decrease in the number of platelets in the blood. Repeated lumbar puncture, if indicated, is performed after 5-7 days. Despite the presence of contraindications, lumbar puncture is performed in cases of papilledema (when purulent meningitis is suspected) and in patients with benign intracranial hypertension.
When is spinal tap prohibited?
Before the procedure, you need to know in what cases lumbar puncture is prohibited.
Absolute contraindications:
- Marked swelling and increase in brain volume.
- Sudden increase in intracranial pressure.
- Neoplasms in brain tissue.
- Closed hydrocephalus is a pathology in which cerebrospinal fluid cannot independently enter the subarachnoid space due to obstacles.
If there are such contraindications, a child or adult is prohibited from having a lumbar puncture. Otherwise, the risk of axial herniation of the brain increases - this is a pathology in which part of the brain is displaced into the foramen magnum. Then the work of vital areas is disrupted, which threatens the death of the patient. Herniation can occur if the doctor uses a thick needle and removes a lot of cerebrospinal fluid from the spinal canal.
Carefully! If a lumbar puncture is necessary, and the likelihood of brain herniation is high, then a minimum amount of cerebrospinal fluid should be extracted. When symptoms of pathology appear, you must immediately inject the required volume of cerebrospinal fluid using a needle.
There are other contraindications for spinal puncture:
- Presence of pustules on the lower back.
- Blood clotting disorder.
- Medicines that thin the blood (antiplatelet agents, anticoagulants).
- Blockade of the subarachnoid space.
- Bleeding due to local dilation and rupture of a vessel (aneurysm) in the brain or spinal cord.
- The period of gestation.
In the presence of such conditions, the doctor decides to perform the procedure, taking into account possible complications.
When is a lumbar puncture necessary and why not?
lumbar puncture
Lumbar puncture is performed both for diagnostic purposes and for therapy, but always with the consent of the patient, except in cases where the latter, due to his serious condition, cannot contact the staff.
For diagnosis, a spinal puncture is performed if it is necessary to examine the composition of the cerebrospinal fluid, determine the presence of microorganisms, fluid pressure and patency of the subarachnoid space.
Therapeutic puncture is needed to evacuate excess cerebrospinal fluid or introduce antibiotics and chemotherapy drugs into the intrathecal space in case of neuroinfection or oncopathology.
The reasons for lumbar puncture are mandatory and relative, when the decision is made by the doctor based on a specific clinical situation. Absolute indications include:
- Neuroinfections - meningitis, syphilitic lesions, brucellosis, encephalitis, arachnoiditis;
- Malignant tumors of the brain and its membranes, leukemia, when CT or MRI cannot make an accurate diagnosis;
- The need to clarify the causes of liquorrhea with the introduction of contrast or special dyes;
- Subarachnoid hemorrhage in cases where non-invasive diagnosis is not possible;
- Hydrocephalus and intracranial hypertension - to remove excess fluid;
- Diseases requiring the administration of antibiotics and antitumor agents directly under the membranes of the brain.
Among the relative ones are pathology of the nervous system with demyelination (multiple sclerosis, for example), polyneuropathy, sepsis, unidentified fever in young children, rheumatic and autoimmune diseases (lupus erythematosus), paraneoplastic syndrome. A special place is occupied by lumbar puncture in anesthesiology, where it serves as a method of delivering an anesthetic to the nerve roots to provide fairly deep anesthesia while maintaining the patient’s consciousness.
If there is reason to suspect a neuroinfection, then the cerebrospinal fluid obtained by puncture of the intrathecal space will be examined by bacteriologists, who will establish the nature of the microflora and its sensitivity to antibacterial agents. Targeted treatment significantly increases the patient's chances of recovery.
With hydrocephalus, the only way to remove excess fluid from the subarachnoid spaces and the ventricular system is puncture, and often patients feel relief almost immediately as soon as cerebrospinal fluid begins to flow through the needle.
If tumor cells are detected in the resulting liquid, the doctor has the opportunity to accurately determine the nature of the growing tumor, its sensitivity to cytostatics, and subsequent repeated punctures can become a way to administer drugs directly to the area of tumor growth.
Lumbar puncture may not be performed on all patients. If there is a risk of harm to health or danger to life, then the manipulation will have to be abandoned. Thus, the following are considered contraindications for puncture:
- Cerebral edema with risk or signs of herniation of brain stem structures or cerebellum;
- High intracranial hypertension, when removal of fluid can provoke dislocation and wedging of the brain stem;
- Malignant neoplasms and other space-occupying processes in the cranial cavity, intracerebral abscesses;
- Occlusive hydrocephalus;
- Suspicion of dislocation of stem structures.
The conditions listed above are fraught with the descent of the stem structures to the foramen magnum with their wedging, compression of vital nerve centers, coma and death of the patient. The wider the needle and the more fluid removed, the higher the risk of life-threatening complications. If the puncture cannot be delayed, then the minimum possible volume of cerebrospinal fluid is removed, but if wedging occurs, a certain amount of liquid is reintroduced.
If the patient has suffered a severe traumatic brain injury, massive blood loss, has extensive injuries, or is in a state of shock, it is dangerous to perform a lumbar puncture.
Other obstacles to the procedure may include:
- Inflammatory pustular, eczematous skin changes at the point of the planned puncture;
- Pathology of hemostasis with increased bleeding;
- Taking anticoagulants and antiplatelet agents;
- Aneurysm of cerebral vessels with rupture and bleeding;
- Pregnancy.
These contraindications are considered relative, increasing the risk of complications, but in cases where puncture is vitally necessary, they can be neglected if maximum caution is observed.
Technique for performing spinal cord puncture
The technique of performing a lumbar puncture is simple, but requires caution and knowledge of anatomy, so it is performed by an experienced doctor with the help of a nurse.
To perform a lumbar puncture, a special needle with a mandrel is used
First, the assistant prepares the kit for the procedure:
- gloves, mask;
- antiseptic solution that contains iodine;
- cotton wool;
- sterile underwear with a hole for the puncture site;
- Beer puncture needle with mandrin (rod for closing the lumen of the needle);
- test tubes with caps;
- adhesive plaster.
The nurse prepares the patient for the procedure and provides care after it.
Important. The main thing during a lumbar puncture is to correctly determine the puncture site. In some pathologies of the spinal column, it is impossible to pierce the spinal canal.
First, the doctor explains all the details of the cerebrospinal fluid (CSF) collection procedure to the patient. In addition, before the manipulation it is necessary to empty the bladder and intestines.
Lumbar puncture in the lateral position
In the ward, the patient must take a lying or sitting position. In the first case, the patient lies on the couch on his side, arching his back and pulling his knees towards his stomach (fetal position). In this position it is easiest to feel all the vertebrae, processes and even the distance between them.
In the second case, the patient sits on the couch and bends his torso forward to make it easier for the doctor to determine the puncture site in the lumbar spine.
Technique for performing lumbar puncture:
Symptoms and prognosis for spinal cord tumor
- The puncture point is determined, which is located between L3 – L4 (third and fourth lumbar vertebrae) or L4 – L5.
- The puncture area is wiped with an antiseptic three times, starting from the intervertebral area and continuing to increase the circumference.
- After the antiseptic has dried, the back is covered with sterile linen with a hole.
- An anesthetic injection is given; as a rule, Novocaine, Lidocaine or Ultracaine are used for this.
- The puncture needle is inserted into the previously determined space between the spinous processes at an angle, trying to adhere to the midline.
- The doctor punctures all layers in turn (for example, the yellow ligament, dura mater) until he penetrates the spinal canal. After passing through all the structures, the needle seems to fall into the spinal canal. If there is no such sensation, then you need to remove the mandrin; if the liquid leaks, then this indicates that the needle is already inside the canal. If the doctor has inserted the needle correctly, but the cerebrospinal fluid does not flow out, the patient is asked to cough or sit up to increase fluid pressure.
- Next, the liquid is collected in different test tubes of approximately 1 ml. The liquid should drain passively; do not extract it with a syringe.
- Then you need to measure the pressure, which is normally 100 - 150 mm Hg. Art. To get accurate results, you need to relax as much as possible. The pressure can be determined approximately: 60 drops of CSF is the norm. During inflammatory processes, the volume of cerebrospinal fluid increases.
- The needle is carefully removed, the puncture site is treated with an antiseptic and a sterile bandage is applied.
During a lumbar puncture, the needle is inserted between the third and fourth lumbar vertebrae at a slightly inclined angle.
The procedure lasts approximately 30 minutes.
Lumbar puncture in newborns has its own characteristics:
- The child is held in a position on his side or sitting so that the lumbar region is flexed. In this case, you need to ensure that the cervical segment does not bend, because then the patency of the upper respiratory tract worsens.
- In very low birth weight premature babies, the puncture is made in the area between the 4th and 5th lumbar vertebrae to avoid damaging the spinal cord.
- The depth of needle insertion is up to 1 – 1.5 cm.
Reference. With numerous lumbar punctures, adhesions appear, due to which the fluid may not flow out. Then the puncture is performed in an area slightly higher or lower.
The spinal puncture protocol is recorded in the medical history.
Algorithm
Neurologists at the Yusupov Hospital perform a lumbar puncture according to the procedure algorithm. The nurse prepares a lumbar puncture kit:
- sterile gloves;
- sterile forceps;
- alcohol (70%) or 0.5% alcohol solution of chlorhexidine for skin treatment;
- adhesive plaster and sterile beads, adhesive plaster;
- 5 syringes with a capacity of 5 ml and needles for them;
- 0.25% or 0.5% solution of novocaine for anesthesia of the puncture site;
- 1-2% trimecaine solution for administration into the subdural and epidural space;
- sterile needles with a mandrel 10-12 cm long (Bier needle for lumbar puncture);
- sterile tubes for collecting cerebrospinal fluid.
The patient is psychologically prepared for lumbar puncture according to the algorithm. Successful spinal puncture largely depends on the correct position of the patient. Immediately before the puncture, the patient is given a fetal position - laid on his side, head tilted as much as possible, legs bent at the hip and knee joints.
At the level of the line that connects the superior posterior iliac spines, the doctor determines the gap between the spinous processes of the third and fourth lumbar vertebrae. Before puncture, the skin is treated with iodine. After this, the iodine is carefully removed with alcohol so that it does not enter the subarachnoid space. The spinal puncture site is surrounded with a sterile drape.
The site of the intended puncture is anesthetized with a 0.5% novocaine solution. A mandrel is inserted into the needle for lumbar puncture, the skin is pierced, and the direction of the needle is specified. As the needle is inserted, the doctor sequentially overcomes the resistance of the ligamentum flavum and dura mater. After puncture of the dura mater, the spinal puncture needle is inserted very slowly. From time to time, the mandrel is removed to check whether cerebrospinal fluid is leaking. When the needle enters the subarachnoid space, a sinking sensation occurs. When cerebrospinal fluid appears, the needle is advanced another 1–2 mm.
The patient is then asked to relax and carefully straighten his legs and head. The doctor removes the mandrin, preventing the cerebrospinal fluid from leaking. A pressure gauge is attached to the needle and the cerebrospinal fluid pressure is measured. It is normally 100–150 mm of water column. The flow of cerebrospinal fluid, if necessary, is increased by coughing, pressing the jugular veins or abdomen, or the jugular veins.
Cerebrospinal fluid is collected in at least 3 sterile tubes:
- firstly, to determine the concentration of glucose and protein;
- in the second - for serological research and determination of the cellular composition of the cerebrospinal fluid;
- in the third - for bacteriological examination of cerebrospinal fluid.
If doctors suspect tuberculous meningitis in a patient, collect cerebrospinal fluid in a fourth tube to identify the fibrin film. After collecting the cerebrospinal fluid, the mandrin is removed and the needle is removed. When a lumbar puncture is performed, the technique used in children has its own peculiarities. In children, the needle is placed perpendicular to the line of the spine, and in adults - slightly at an angle, open in the direction of the horse's tail.
Feelings during the procedure
Many patients are interested in the question of whether it is painful to perform a lumbar puncture. If the procedure is performed correctly, the patient does not feel any significant discomfort or pain. He can feel the needle passing through the hard membranes, but there is no painful reaction. Unpleasant symptoms do not appear, since the doctor administers an anesthetic solution before the puncture.
You may feel an electric shock if the needle hits a spinal nerve. Some patients experience headaches during the procedure.
[node:field_similarlink]
Rules of conduct after puncture
It is recommended to lie on your stomach for 3 hours after a lumbar puncture. It is also prohibited to lift heavy objects or subject yourself to physical stress. If these rules are followed, the patient will be able to avoid leakage of cerebrospinal fluid from the hole.
If medications are administered into the subarachnoid space, the patient must remain in bed for at least 3 days.
Carefully. If there is an increase in temperature, numbness or fluid discharge from the hole after the puncture, you should visit a doctor.
Research results
As a rule, CSF is collected in 3 containers, which are then sent for general, biochemical and microbiological analysis.
Doctors pay attention to the color of the cerebrospinal fluid:
- Bloody - an admixture of blood in the fluid may indicate blood leaking into the cavity between the arachnoid and pia mater.
- The yellowish color of the CSF indicates long-term development of hemorrhagic processes, for example, subdural hematoma (accumulation of blood between the brain and membranes), metastases in the meninges, blockage of the cerebrospinal fluid pathways.
- Grayish-green – neoplasms in the brain.
- Transparent – the person is healthy.
The ventricular mass is carefully examined, doctors measure pressure, determine the amount of protein, glucose, etc.
Normal results of a cerebrospinal fluid test look like this:
- liquid color – transparent;
- protein level – from 150 to 450 mg/l;
- glucose concentration – from 4 to 60% of the blood level;
- there are no atypical cells;
- leukocytes – up to 5 in 1 mm³ of blood;
- neutrophils and red blood cells are absent;
- pressure – from 150 to 200 mm Hg. Art.
Important. If the cerebrospinal fluid pressure is higher than normal, then decongestant therapy should be performed. If this indicator is underestimated, then this indicates brain pathologies.
Red blood cells, neutrophils and pus indicate blood diseases. Atypical cells are found in brain tumors, and sugar levels decrease in bacterial meningitis.
Lumbar puncture will allow timely identification of many dangerous diseases and treatment.
No ads 3
How to take a puncture
The sequence of actions when performing a spinal puncture is as follows:
- The patient is placed on his side and asked to press his knees to his stomach and tilt his head. This position allows you to expand the spaces between the vertebrae for unhindered penetration of the needle. In some cases, the procedure is performed in a sitting position with a rounded back.
- The health worker selects the puncture site: this is the space between the 3rd and 4th or 4th and 5th lumbar vertebrae. In this place, the risk of damage to nerve tissue is eliminated, since the spinal cord ends higher.
- The skin in this area is treated with an antiseptic.
- Using a regular syringe with a thin needle, local anesthesia is performed with a solution of novocaine or lidocaine.
- After the anesthetic has taken effect, a puncture needle can be inserted. This is a special needle, 7-10 cm long, with a large clearance of 4-6 mm. The lumen of the needle is closed by a mandrin - this is a metal rod inside the needle, which is removed only when it enters the subarachnoid space of the spinal cord. The mandrin ensures the cleanliness of the needle lumen - it does not become clogged with tissue.
- During the puncture process, the needle is directed almost at a right angle to the body, pointing slightly upward. At a depth of 5-6 cm in adults or 2 cm in children, a “needle drop” is felt - tissue resistance disappears. This means that the needle entered the subarachnoid space where cerebrospinal fluid circulates.
- The mandrin is removed, and a container for collecting cerebrospinal fluid or a syringe is placed at the outer end of the needle. Normally, cerebrospinal fluid drips slowly from the needle. In cases of a strong increase in intracranial pressure, it can flow out in a stream under pressure.
- When enough cerebrospinal fluid has been drawn, the needle is slowly withdrawn. The needle insertion site is once again treated with an antiseptic and a cotton swab with collodion is applied. Collodion is a film-forming preparation (so-called skin glue).
Important. At the end of the procedure, the patient is left in a supine position for several hours.
this helps the body stabilize cerebrospinal fluid pressure and recover from shock.
Some patients (especially those who have problems with the nervous system) may react to the puncture as follows:
- general weakness
- headache,
- back pain,
- nausea (with possible vomiting),
- urinary retention.
If the procedure is carried out for the purpose of anesthesia, then a syringe with novocaine is attached to the needle and slowly, as the needle moves through the tissue, it is injected for pain relief.
The bulk of the anesthetic is injected into the subarachnoid space to temporarily block the sensory nerve fibers that approach the spinal cord.
Laboratory examination of cerebrospinal fluid
Analysis of cerebrospinal fluid begins from the moment it flows out of the needle. The ideal speed is 1 drop per second. If this indicator is elevated, then we can talk about increased intracranial pressure.
For reference. Next, the clarity of the cerebrospinal fluid, the presence of sediment and odor are assessed. Normally, cerebrospinal fluid will be in the form of distilled water. Some diseases of bacterial etiology lead to turbidity of the cerebrospinal fluid and the appearance of a sharp purulent odor (meningitis, encephalitis).
In the presence of pathology, the fluid may acquire a yellowish tint (this color is characteristic of the disease xanthochromia) or become cloudy (this is characteristic of inflammation of the meninges).
Various types of laboratory research are carried out on the selected material:
- biochemical analysis - allows you to evaluate the composition of the fluid and detect pathological components;
- bacteriological culture - makes it possible to detect the presence of microorganisms in the cerebrospinal fluid (normally it should be sterile);
- immunological analysis - checking for the presence of leukocytes in the cerebrospinal fluid (immune cells).
For reference. The data from these studies confirm or refute the proposed diagnosis. With such information, the doctor can prescribe or adjust treatment for the patient.
Complication of spinal cord puncture
Consequences of puncture are rare (in 1–5 patients out of 1000):
- displacement and herniation of brain tissue;
- the appearance of symptoms of meningitis due to irritation of the meninges;
- neuroinfections as a result of violation of antiseptic rules by doctors;
- severe headache may be associated with impaired CSF circulation;
- severe pain along a certain nerve when the spinal cord roots are damaged;
- hemorrhages due to bleeding disorders or taking medications that thin the blood;
- epidermoid cyst;
- meningeal reaction - changes in CSF parameters after the administration of medications or contrast solutions.
These are the main complications that can occur after a lumbar puncture.
Complications
The most serious consequence of lumbar puncture is herniation. It can develop in patients with a volumetric process of the brain against the background of intracranial hypertension. With a sudden drop in pressure in the spinal canal, the uncus of the hippocampus becomes wedged into the notch of the tentorium of the cerebellum or the cerebellar tonsils into the foramen magnum or. If the cerebrospinal fluid pressure turns out to be high, only a minimal amount of cerebrospinal fluid is removed for examination, mannitol and glucocorticoids are prescribed, and the patient is monitored. If there is a high risk of herniation or deterioration of the patient’s condition during lumbar puncture, the needle with the inserted mandrin is left in place, mannitol and high doses of corticosteroids are administered intravenously, after which the needle is removed. Complete or partial blockade of the subarachnoid space, caused by compression of the spinal cord, can cause herniation of the spinal cord with rapidly increasing focal symptoms.
Headaches after lumbar puncture occur in 10-30% of patients. They are associated with prolonged leakage of cerebrospinal fluid through a hole in the dura mater, which leads to a decrease in intracranial pressure. The pain is most often localized in the occipital and frontal region and occurs in the first three days after the puncture. How many days do you have a headache after a lumbar puncture? The headache usually lasts 2-5 days, but sometimes lasts for several weeks.
Back pain after lumbar puncture is associated with damage to the spinal cord roots. Sometimes there is a transient lesion of the abducens nerve, accompanied by the appearance of paralytic convergent strabismus and double vision. If the needle passes through infected tissue, meningitis may develop. Local complications of lumbar puncture in the form of redness at the puncture site are rare and do not require treatment.
Doctors at the Neurology Clinic will perform a lumbar puncture. Get a consultation with a neurologist by first making an appointment by phone at the Yusupov Hospital.
Cost of the procedure
Prices for spinal puncture depend on the level of the clinic, the complexity and nature of the procedure.
In Moscow, the cost of lumbar puncture differs depending on the medical institution:
- Clinic "El. En." — 5400 rubles.
- "PENTA-CLINIC" - 3350 rubles.
- Medical - 2300 rubles.
- Central Clinical Hospital No. 2 of JSC Russian Railways - 1,700 rubles.
- Clinical Hospital No. 119 – 1500 rubles.
- Children's Clinical Hospital named after Semashko - 1450 rubles.
The higher the qualifications of the doctors, the better the equipment of the medical facility and the more complex the procedure, the more you will have to pay for it.
Contraindications for lumbar puncture
If there is a real suspicion of intracranial hematoma or post-traumatic brain abscess (especially temporal localization), lumbar puncture should be avoided.
In comatose patients, lumbar puncture is permissible only when the etiology of the coma is unclear and its differential diagnosis is necessary:
- alcoholic coma
- traumatic coma
- vascular coma
- intoxication coma
- diabetic coma, etc.
If there are signs of brain stem entrapment in the tentorial or foramen magnum in the TBI clinic, lumbar puncture is contraindicated.
With combined TBI, additional contraindications to lumbar puncture often arise:
- traumatic shock
- massive blood loss
- extensive damage to the soft tissues of the back
Lumbar puncture should not be done for bedsores and suppurative processes in the lumbosacral region.
Complications that may occur during lumbar puncture include meningism.
When performing a lumbar puncture with compression of the brain, a life-threatening symptom complex of descending herniation of the brain stem may develop due to a decrease in hydraulic support at the spinal level.
Reviews
Almost all patients respond positively to lumbar puncture. The procedure does not cause significant discomfort or pain, but provokes mental stress. In most cases, there are no complications after a lumbar puncture, although it all depends on the skill level of the doctor.
Irina, 45 years old: “I was treated several times in an inpatient setting for meningitis, and then a lumbar puncture was prescribed. It was scary the first time, but then I realized that there was nothing wrong with it. I felt a slight pain only during the anesthetic injection, then there was a sensation of interference in the lower back, but it became numb. The main thing is to find an experienced doctor, because you can remain disabled if you catch a nerve.”
Ekaterina, 34 years old: “I had a lumbar puncture twice for suspected meningitis. There were no serious complications after the procedure, although after the first time I had a headache. The second time I asked the doctor to make a puncture with a smaller needle, then I didn’t feel anything at all, and there was no headache.”
Igor, 44 years old: “I had to do a spinal tap 3 times. During the procedure, pain is not felt, only movement in the lumbar region was heard, this causes psychological discomfort. I tried to distract myself and stopped paying attention to it. There were never any complications after the study.”
Evaluation of the result of spinal puncture
The result of a cytological analysis of the cerebrospinal fluid is ready on the day of the study, and if bacteriological culture and assessment of the sensitivity of microbes to antibiotics is necessary, the wait for an answer can last up to a week. This time is necessary for microbial cells to begin to multiply in nutrient media and show their response to specific drugs.
Normal cerebrospinal fluid is colorless, transparent, and does not contain red blood cells. The permissible amount of protein in it is no more than 330 mg per liter, the sugar level is approximately half of that in the patient’s blood. It is possible to find leukocytes in the cerebrospinal fluid, but in adults the norm is considered to be up to 10 cells per µl, in children it is slightly higher depending on age. Density is 1.005-1.008, pH - 7.35-7.8.
An admixture of blood in the cerebrospinal fluid indicates hemorrhage under the membranes of the brain or injury to the vessel during the procedure. To distinguish between these two reasons, the liquid is taken into three containers: in case of hemorrhage, it is colored homogeneously red in all three samples, and in case of damage to the vessel, it becomes lighter from the 1st to the 3rd tube.
The density of cerebrospinal fluid also changes with pathology. So, in the case of an inflammatory reaction, it increases due to the cellularity and protein component, and in case of excess fluid (hydrocephalus) it decreases. Paralysis, brain damage from syphilis, and epilepsy are accompanied by an increase in pH, and with meningitis and encephalitis it falls.
The cerebrospinal fluid may darken with jaundice or metastases of melanoma, it turns yellow with an increase in the content of protein and bilirubin, after a previous hemorrhage under the membranes of the brain.
Cloudiness of the cerebrospinal fluid is a very alarming symptom that may indicate leukocytosis due to bacterial infection (meningitis). An increase in the number of lymphocytes is typical for viral infections, eosinophils for parasitic infestations, and erythrocytes for hemorrhages. The protein content increases with inflammation, tumors, hydrocephalus, infectious damage to the brain and its membranes.
The biochemical composition of the cerebrospinal fluid also indicates pathology. Sugar levels decrease with meningitis and increase with strokes, lactic acid and its derivatives increase in the case of meningococcal lesions, abscesses of brain tissue, ischemic changes, and viral inflammation, on the contrary, leads to a decrease in lactate. Chlorides increase with neoplasms and abscess formation, and decrease with meningitis and syphilis.
According to reviews from patients who have undergone a spinal puncture, the procedure does not cause significant discomfort, especially if it is performed by a highly qualified specialist. Negative consequences are extremely rare, and patients experience the main concern at the stage of preparation for the procedure, while the puncture itself, performed under local anesthesia, is painless.
Main conclusions
As you can see, lumbar puncture is an important and also informative diagnostic and treatment procedure. Most often it is prescribed for neuroinfections, suspected subarachnoid bleeding, malignant process, autoimmune pathologies of the nervous system. It is contraindicated in cases of severe cerebral edema, a sharp increase in intracranial pressure, the presence of a large tumor in the brain, etc. There are some features of performing a lumbar puncture for children and adults. To ensure that the procedure goes without complications, you need to contact an experienced specialist. After a lumbar puncture, the cerebrospinal fluid is sent for research, during which dangerous diseases of the nervous system can be identified and treated. Most patients who have had a lumbar puncture are satisfied with its results; they claim that there is no discomfort or pain during it.
1 What is a spinal tap and why is it done?
A lumbar puncture (also known as a spinal puncture or lumbar puncture) is a diagnostic procedure performed to collect cerebrospinal fluid for subsequent analysis.
The procedure technique involves inserting a special needle into the subarachnoid space of the spinal cord exclusively at the level of the lumbar spine. In some cases, manipulation is not carried out for diagnostic purposes, but for therapeutic or anesthetic purposes.
- How to take a puncture
- Indications for spinal cord puncture
- Types of puncture in gynecology
- Technique for performing cerebrospinal fluid puncture
- Consequences of puncture
- Basic information
- Evaluation of the result of spinal puncture
- Technique for performing spinal cord puncture
- Goals of the study and indications for the procedure
Lumbar puncture is performed in the lumbar region
But why is it made specifically? Why is it needed and what does it show? As a rule, a lumbar puncture is required in cases where it is necessary to exclude severe diseases of the central nervous system. For example, meningitis, encephalitis or even cancer.
1.1 Indications for lumbar puncture
Indications for lumbar puncture should be differentiated, dividing them into diagnostic and therapeutic/manipulative (in the latter case we are talking about the administration of painkillers).
Diagnostic indications include:
- To identify meningitis (viral, bacterial).
- For the purpose of identifying neurosyphilis, encephalitis (of any etiology).
- Confirmation or refutation of the patient's bleeding into the central nervous system.
- In order to identify demyelinating pathologies (for example, multiple sclerosis).
- In order to detect malignant primary tumors of the central nervous system or metastases of secondary tumors.
Therapeutic/manipulative indications include:
- for medicinal purposes - for the administration of antimicrobial drugs or chemotherapy drugs;
- for manipulation purposes - to reduce increased intracranial pressure of various etiologies;
- for analgesic purposes - for the administration of analgesic/analgesic medications.
1.2 Are there any contraindications?
There are a number of absolute and relative contraindications to performing a lumbar puncture. Relative contraindications vary from patient to patient, that is, there is no exact list of them.
Lumbar puncture in children
Absolute contraindications include:
- Extremely high intracranial pressure (greater than 220 millimeters H2O).
- Septic lesions (generalized infection, infection with pathogenic blood flora).
- Local infectious processes in the injection area.
- Massive bleeding of any organs of the body (including the central nervous system).
- The presence of severe deformities of the spinal column (scoliosis, pathological kyphosis or lordosis, spinal adhesions).
- The patient has intracranial expansive processes.
1.3 What can a spinal tap determine?
The diseases described in the previous paragraph can be confirmed by a thorough analysis of the cerebrospinal fluid (CSF) taken during the procedure. But how are the results analyzed after the procedure?
Using special instruments (a set of reagents, microbiological equipment), cerebrospinal fluid is assessed according to the following criteria:
- Cerebrospinal fluid pressure is measured (directly during the procedure);
- the cerebrospinal fluid is assessed using a macroscopic method;
- the amount of proteins and sugar in the liquor is analyzed;
- The cellular morphology of the obtained cerebrospinal fluid is analyzed.
CSF collection during lumbar puncture
After all the described manipulations, the final verdict is made: normal or pathological. However, diagnosticians do not make a diagnosis; they only state the norm or deviation based on the results. The diagnosis is made by the attending physician.
1.4 Norm and deviations
Whether the cerebrospinal fluid is normal is judged by several criteria, including its color. Liquor can have four different colors:
- Bloody color - there are hemorrhagic pathological processes (most often early-stage subarachnoid hemorrhage).
- Yellowish color - late stage of hemorrhagic pathological processes (for example, carcinomatosis, blockage of the cerebrospinal fluid circulation, chronic hematomas).
- Grayish-green color - in most cases indicates the presence of malignant brain tumors.
- Transparency is the absolute norm.
Patient position for lumbar puncture
Biochemical parameters of the cerebrospinal fluid are also assessed. The norm is:
- color: transparent;
- amount of protein: 150-450 milligrams per liter;
- amount of glucose (sugar): from 60% in the blood;
- atypical cells: absent;
- leukocytes: no more than 5 mm3;
- neutrophils: absent;
- red blood cells: absent;
- liquor pressure is within 150-200 water column or 1.5-1.9 kPa.