Tumors of the pineal gland parenchyma are tumor formations of the brain that arise in the parenchyma of the pineal gland, which have the form of a dense node of gray-red color and are located in the posterior parts of the third ventricle (the so-called pineal region). Pinealomas account for about 30% of the total number of tumors of the pineal gland parenchyma.
Causes of the disease
Tumors of the pineal gland are rare and affect people mainly in adolescence (13-20 years).
Classification of pineal gland tumors:
- Pineocytoma is a slow-growing tumor that consists of mature pinealocytes. It is observed in approximately 45% of patients with tumors of the pineal gland. Develops at the age of 25-30 years equally often in men and women.
- Pineoblastoma is a high-grade tumor. Accounts for about 45% of all pineal gland tumors. Has a tendency to metastasis. It is detected mainly in adolescence (childhood), although it is very rare in adults.
- A tumor of the pineal gland parenchyma is characterized by the least predictable course. They are more often observed in adults and account for only 10% of all tumors of the pineal gland.
Symptoms and course of the disease
The type and location of the pineal affects symptoms. The slow growth of pineocytoma causes a gradual increase in symptoms with a generally satisfactory condition, while with pineoblastoma there is rapid development and a sharp deterioration in the patient’s condition.
Due to compression of the posterior part of the third ventricle and the cerebral aqueduct, symptoms associated with increased intracranial pressure, hydrocephalus and midbrain syndrome (oculomotor disorders) occur:
- headache;
- attacks of nausea and vomiting;
- fatigue, weakness, drowsiness;
- visual disturbances: deterioration of the pupil's reaction to light, double vision;
- memory impairment;
- hearing disorders;
- violations of oral and written speech;
- cerebellar disorders: unstable statics and difficulty walking;
- weight loss or gain.
The presence of neurological symptoms (including spinal) indicates the development of metastases in the spinal cord.
Treatment of the disease
The choice of therapy is determined by the histology of the diagnosis. The main treatment method for parenchymal tumors is surgery, during which complete or maximum possible removal of the tumor is performed.
For pineocytoma, radical removal of the tumor is resorted to.
For pineoblastoma, excision of the tumor is performed to the maximum extent possible in combination with irradiation of both the brain and spinal cord.
For a tumor of the pineal parenchyma of intermediate differentiation, therapeutic therapy is carried out by analogy with that used for pineoblastoma.
For parenchymal tumors in children under 3 years of age, chemotherapy is used, and for children over 3 years of age, radiation therapy is used. In case of hydrocephalus, ventriculoperitoneal shunting or endoscopic ventriculostomy of the third ventricle is necessary.
With pineocytomas, radical excision of the tumor ensures a cure for the patient.
Partial tumor removal helps achieve 85% 5-year survival rate.
Comprehensive and adequate treatment for pineoblastoma helps to achieve 5-year survival in 58% of cases and 3-year survival in 78% of cases.
The prognosis for intermediate-grade pineal parenchyma tumors is similar to that for pineoblastoma.
Treatment
As in the case of oncological diseases of other organs, the greatest effectiveness in the treatment of tumors of the pineal gland is shown by an integrated approach, which involves the combination of several methods of therapy at the same time.
Radiosurgical treatment with the CyberKnife system
Treatment of brain tumors using the CyberKnife system
If the tumor of the pineal gland is small, the patient may be recommended radiosurgery using CyberKnife. This innovative cancer treatment method, which allows the treatment of brain tumors without surgery, has proven its effectiveness all over the world. Unlike traditional neurosurgery, CyberKnife radiosurgery does not require craniotomy, which, combined with the precision of delivering thin beams of radiation, significantly reduces the risk of damage to healthy tissues of this vital organ.
The radiosurgical treatment method involves delivering a high dose of ionizing radiation precisely to the boundaries of the tumor. As a result of receiving high doses of radiation, tumor cells die, and healthy tissues around the tumor focus remain maximally protected - a high dose is formed in the areas of intersection of thin radiation beams, which are specified according to a three-dimensional digital model of the location of the tumor and surrounding structures.
As a rule, radiosurgery of pineal tumors includes one or two sessions lasting up to half an hour, during which the patient remains conscious and can independently leave the clinic at the end of treatment.
Pineal gland tumor: treatment plan using the CyberKnife system
Bloodless, painless, no need for anesthesia, reduced risk of irreparable neurological damage - in comparison with surgical intervention in the deep structures of the brain, CyberKnife treatment allows the patient to carry out treatment on an outpatient basis, without interruption from the daily schedule of his life.
Surgery
The use of CyberKnife in the treatment of brain tumors is not always possible, since there is a limitation on the size of the tumor for radiosurgery.
Therefore, in the case of a large volume of brain tumor, the main treatment method will be surgery. Surgery for brain tumors involves minimally invasive surgery. During the operation, a sample of tumor tissue is taken for histological examination, and the maximum possible volume of the tumor is removed, so that no damage is caused to healthy brain tissue.
Radiation therapy
The modern Elekta linear accelerator with IMRT function allows for gentle radiation therapy with simulated ionizing radiation dose intensity
However, if the tumor is localized in a place of the brain that is difficult to access for surgical intervention, only part of the tumor is removed during surgery, and then the treatment is supplemented with a course of radiation therapy and the use of modern chemotherapy drugs, including to counteract possible metastases of brain cancer.
Radiation therapy for brain tumors is carried out on a high-precision linear accelerator Electa Synergy, equipped with an IMRT system (modeled by the intensity of ionizing radiation dose delivery). This makes it possible to significantly increase the accuracy and safety of treatment, as well as reduce the duration of each radiation therapy session, in contrast to treatment using linear accelerators of outdated models and cobalt devices.
IMRT allows high doses of ionizing radiation to be delivered precisely to the tumor boundaries with minimal impact on nearby healthy brain tissue.
Radiation therapy is also widely used for palliative treatment in cases where the tumor is incurable (multiple brain metastases, large tumor volume affecting critical brain structures, etc.). In this case, radiation therapy can reduce the severity of symptoms and improve the patient’s quality of life.
Prices
| Disease | Approximate price, $ |
| Prices for thyroid cancer screening | 3 850 — 5 740 |
| Prices for examination and treatment for testicular cancer | 3 730 — 39 940 |
| Prices for examinations for stomach cancer | 5 730 |
| Prices for diagnosing esophageal cancer | 14 380 — 18 120 |
| Prices for diagnosis and treatment of ovarian cancer | 5 270 — 5 570 |
| Prices for diagnosing gastrointestinal cancer | 4 700 — 6 200 |
| Prices for breast cancer diagnostics | 650 — 5 820 |
| Prices for diagnosis and treatment of myeloblastic leukemia | 9 600 — 173 000 |
| Prices for treatment of Vater's nipple cancer | 81 600 — 84 620 |
| Prices for treatment of colorectal cancer | 66 990 — 75 790 |
| Prices for treatment of pancreatic cancer | 53 890 — 72 590 |
| Prices for treatment of esophageal cancer | 61 010 — 81 010 |
| Prices for liver cancer treatment | 55 960 — 114 060 |
| Prices for treatment of gallbladder cancer | 7 920 — 26 820 |
| Prices for treatment of stomach cancer | 58 820 |
| Prices for diagnosis and treatment of myelodysplastic syndrome | 9 250 — 29 450 |
| Prices for leukemia treatment | 271 400 — 324 000 |
| Prices for thymoma treatment | 34 530 |
| Prices for lung cancer treatment | 35 600 — 39 700 |
| Prices for melanoma treatment | 32 620 — 57 620 |
| Prices for treatment of basal cell carcinoma | 7 700 — 8 800 |
| Prices for the treatment of malignant skin tumors | 4 420 — 5 420 |
| Prices for treatment of eye melanoma | 8 000 |
| Prices for craniotomy | 43 490 — 44 090 |
| Prices for thyroid cancer treatment | 64 020 — 72 770 |
| Prices for treatment of bone and soft tissue cancer | 61 340 — 72 590 |
| Prices for treatment of laryngeal cancer | 6 170 — 77 000 |
| Testicular cancer treatment prices | 15 410 |
| Bladder cancer treatment prices | 21 280 — 59 930 |
| Prices for cervical cancer treatment | 12 650 — 26 610 |
| Prices for treatment of uterine cancer | 27 550 — 29 110 |
| Prices for treatment of ovarian cancer | 32 140 — 34 340 |
| Prices for treatment of colon cancer | 45 330 |
| Prices for lymphoma treatment | 11 650 — 135 860 |
| Prices for kidney cancer treatment | 28 720 — 32 720 |
| Prices for breast reconstruction after cancer treatment | 41 130 — 59 740 |
| Prices for breast cancer treatment | 26 860 — 28 900 |
| Prices for prostate cancer treatment | 23 490 — 66 010 |
Symptoms of pineal tumors
The pineal gland measures up to 12 mm in length, 3-8 mm in width and 4 mm in thickness, and its weight varies from 0.1 to 0.18 g. The pineal gland, as an endocrine organ, influences many processes in the body. The gland produces about 40 active compounds, which include melatonin and serotonin. In addition, the organ affects age-related and gender-related changes in the human body.
A tumor in the pineal gland can grow to be as large as the gland itself—or even larger.
Due to the growth of the tumor, a headache occurs, leading to nausea and sometimes vomiting.
The tumor compresses the pineal gland and the cerebrospinal fluid pathways of the brain, which in turn causes hydrocephalus—an accumulation of fluid inside the brain. Hydrocephalus puts pressure on the brain and increases the size of the ventricles. Over time, constant pressure on the brain causes swelling and death of nerve structures, in particular the optic nerves, which leads to poor vision.
The following symptoms may also indicate the presence of a tumor:
- lack of coordination and unsteady gait,
- weakening of muscles,
- hand trembling,
- vertical gaze palsy - inability to move the eyes up or down,
- fast weight loss,
- jumps in body temperature.
What can you say about benign bone tumors and their treatment?
The most common benign bone tumors are non-osteogenic fibroma, simple bone cyst, osteochondroma, giant cell tumor, cartilaginous tumor, and fibrous dysplasia. Since treatment for benign bone tumors depends on the type of tumor and the age of the patient, monitoring the patient is sufficient in most cases. In some cases, drug treatment relieves pain. In some cases, especially in pediatric patients, tumors may disappear spontaneously over time. Some benign tumors can develop into malignant tumors and then metastases may begin to develop. Sometimes the doctor recommends removing the tumor. This approach prevents possible pathological fractures. Some tumors may recur even though they have been excised. Giant cell tumor is the most common benign tumor, which can have an aggressive course of development. In some cases, osteochondroma, which is localized in several areas, can develop into cancer.
BE ATTENTION TO THESE SYMPTOMS!
Specialist in orthopedics and traumatology, Professor Kaan Erler says: “If you experience pain despite being rested or if you suspect a bone tumor, please consult a doctor immediately. Orthopedic oncologists will help you in any situation.”
Clinical picture
Clinical manifestations of pineoblastoma can be headache mainly in the morning (70%), nausea and vomiting, double vision (50%), hearing loss (30%), weakness, sensory disturbance in one half of the body, epileptic seizures, drowsiness (50%) , behavioral disturbances, weight loss/gain (20%). Hypertensive-hydrocephalic crises are possible.
A neurological examination of the patient reveals a general cerebral syndrome, decreased photoreaction of the pupils, vertical gaze paresis, changes in convergence, hypoacusia, hypotonia, coordination disorders, ataxia, and emotional-volitional disorders.
Thyroid tumors
The thyroid gland is located on the front surface of the neck. In most people it can be seen or felt. The thyroid gland has two lobes connected by a narrow isthmus. This gland absorbs iodine from food and blood and produces a hormone that performs various functions. The thyroid gland contains mainly two types of cells: Follicular cells, which produce and store thyroid hormone. In addition, they produce a special protein called thyroglobulin and cells that produce another hormone, calcitonin. From these cells, various types of cancer arise, differing in course, treatment and outcome.
Various tumors arise in the thyroid gland, and most of them (about 95%) are benign. Due to the fact that the thyroid gland is located close to the skin, the tumor that arises in it looks like a node on the neck. Nodules in the gland can appear at any age; they are more often detected in adults who themselves discover a tumor.
Malignant thyroid tumors Only 5-10% of thyroid tumors are malignant. There are several types of thyroid cancer:
Papillary carcinoma accounts for 80-85% of the total number of malignant thyroid tumors. The tumor grows very slowly and usually occurs in one lobe of the gland, but in 10-20% of patients the lesion is bilateral. Although this tumor grows slowly, it often affects the cervical lymph nodes. Fortunately, most people with papillary thyroid cancer recover.
Follicular carcinoma is the second most common malignant tumor of the thyroid gland and accounts for 5-10% of all thyroid tumors. It is more often detected in countries where there is a lack of iodine in food. This type of cancer usually does not spread beyond the thyroid gland, but can sometimes metastasize to the lungs and bones. Unlike papillary carcinoma, follicular carcinomas rarely involve the lymph nodes. The prognosis of patients with follicular carcinoma is the same or slightly worse than that of patients with papillary carcinoma.
Anaplastic carcinoma is a rare type of malignant tumor of the thyroid gland. The tumor quickly affects the structures of the neck and spreads throughout the body, most often leading to death.
Medullary thyroid carcinoma is the only tumor arising from C cells and accounts for 5% of the total number of thyroid malignancies. It can affect the lymph nodes, lungs and liver even before the primary lesion is identified. This tumor produces the hormone calcitonin and carcinoembryonic antigen, which can be detected in the patient’s blood.
Thyroid lymphoma How common is thyroid cancer? At the age of 30 - 39 years, women get sick 7 times more often than men. The maximum incidence of thyroid cancer occurs at the age of 50-59 years. Over the 10-year period from 1993 to 2002, there was an increase in the incidence of thyroid cancer. High morbidity rates among the male population were identified in the Bryansk, Oryol, Saratov regions, Altai Territory, and Krasnodar Territory. The Altai Territory, Bryansk Region, Krasnodar Territory, and Sakhalin Region lead in the incidence rate among women.
What Causes Thyroid Cancer? Much progress has been made in understanding how changes in a person's DNA can turn normal thyroid cells into cancerous ones. DNA is a molecule that carries information about the activities of all cells in the body. We tend to resemble our parents as they are the sources of our DNA. However, DNA affects more than just our appearance. It also determines the risk of developing certain diseases, including cancer.
Some genes (parts of DNA) control cell growth and division. Genes that promote cell division are called oncogenes. Other genes slow down cell division or cause cell death and are called tumor suppressor genes. Neoplasms can arise as a result of mutations (changes) of genes and their effects on oncogenes and tumor suppressor genes.
People can inherit damaged DNA from a parent. In many cases, a person's DNA is damaged by environmental factors such as smoking or radiation. Sometimes DNA mutations occur for unknown reasons.
The DNA mutations that cause some forms of papillary thyroid cancer involve specific parts of the RET oncogene. These mutations are acquired during life and are less likely to be inherited. They are present only in tumor cells and are not transmitted to the patient’s children. Acquired changes in other oncogenes and tumor suppressor genes (eg, ras, trk, gsp, p53) also play a role in the development of papillary and follicular thyroid cancer.
Mutations in patients with medullary thyroid cancer involve different parts of the RET gene (compared to papillary cancer). Almost all patients with a hereditary form of medullary thyroid cancer, and 1 in 5 cases of sporadic forms of the same cancer have a mutation in the RET gene. Most patients with sporadic medullary thyroid cancer have acquired mutations that are present only in their tumor cells. Patients with familial medullary cancer inherit the RET gene mutation from a parent. These mutations are present in every cell of the body and can be detected by examining the DNA of blood cells.
Risk Factors for Thyroid Cancer A risk factor is something that makes you more likely to develop cancer. For example, intense exposure to sunlight on the skin is a risk factor for skin cancer. Smoking is a risk factor for tumors of the lungs, oral cavity, larynx, bladder, kidneys and some other organs. However, the presence of one or more risk factors does not mean that a person will definitely develop cancer.
To date, several factors are known that increase the likelihood of thyroid cancer. However, most people with thyroid cancer do not have obvious risk factors. In addition, many people with one or more risk factors do not develop thyroid cancer at all. If a person has one or more risk factors, it is impossible to draw a conclusion about how much a certain factor influences the occurrence of cancer
Low iodine content in food. Papillary and follicular thyroid cancer is more common in areas of the world where dietary iodine is low. In some countries, iodine is specifically added to table salt and other foods.
Radiation. A proven risk factor for papillary thyroid cancer is childhood head and neck irradiation. In the past, children received radiation for acne, a fungal infection of the scalp, an enlarged thymus gland, and to shrink the size of the tonsils or adenoids. Within a few years, this type of treatment was associated with an increased risk of thyroid cancer. Radiation exposure in adults is associated with a small risk of developing thyroid cancer.
A number of studies have shown that an increased risk of thyroid nodules and even cancer is associated with radioactive fallout from nuclear weapons testing or incidents at nuclear power plants. Thus, there has been an increase in cases of thyroid cancer among children near the Ukrainian city of Chernobyl, where a nuclear power plant exploded in 1986. At the same time, millions of people were exposed to radioactive fallout. First responders and people living near the scene of the incident also have an increased incidence of thyroid cancer, even though they were already adults at the time of the accident.
Hereditary conditions. People with certain inherited diseases also have an increased risk of developing thyroid cancer. Thus, Gardner's syndrome and familial polyposis are accompanied by an increased risk of thyroid cancer. The rare genetic disease Cowden is also associated with an increased risk of thyroid cancer.
20% of medullary thyroid cancers are the result of an inherited altered gene - familial medullary thyroid carcinoma.
Gender and age. Benign thyroid nodules occur more often in women than in men. Most cases of papillary and follicular cancer are detected between the ages of 30 and 50 years. Benign and malignant thyroid tumors can occur in people of all ages.
Lifestyle risk factors. Tobacco products and alcohol are the main risk factors for most head and neck tumors, including tumors of the oral cavity, pharynx, and esophagus. On the other hand, it has not been proven that these factors increase the risk of developing thyroid cancer.
Can thyroid cancer be prevented? Most people with thyroid cancer have no known risk factors, so it is impossible to prevent the vast majority of people from developing the disease. Some researchers believe that the increase in thyroid cancer cases may be explained by X-ray examinations of young children. This assumption has not been confirmed, however, radiological examinations in children should be avoided whenever possible.
Most familial cases of medullary thyroid cancer can be prevented by genetic blood testing. If such a disease is detected in a family, other family members should be examined.
If there is a family history of medullary thyroid cancer, other family members should be seen by a doctor who is up-to-date on genetic counseling and testing. If RET gene mutations are associated with familial medullary thyroid cancer (even if there are no obvious nodules in the gland or other symptoms of the disease), then surgery may be offered to prevent medullary thyroid cancer from occurring. The only way to prevent medullary thyroid cancer in the presence of RET gene mutations is to remove the entire gland. After surgery, hormone replacement therapy is necessary.
Is early detection of thyroid cancer possible? In many cases, thyroid cancer can be detected in the early stages. In fact, in most patients, cancer of this location is diagnosed at an earlier stage, and therefore treated more effectively. In rare cases, thyroid cancer is not accompanied by symptoms and is therefore detected in late stages. Thyroid tumors are diagnosed early if the patient consults a doctor immediately after noticing it. Many tumors are detected during regular preventive examinations.
If unusual symptoms appear in the form of a tumor node on the neck or swelling of the neck, you should immediately see a doctor. Some researchers recommend performing a neck self-examination twice a year to look for unusual lumps or lumps.
People with a family history of medullary thyroid cancer have a very high risk of developing this type of cancer. Removing the thyroid gland in children in such families is an effective method of preventing this type of cancer, which can be fatal. If a patient refuses genetic testing or surgery to prevent medullary thyroid cancer, there are other methods that can help detect cancer at an early stage and provide effective treatment.
Diagnosis of thyroid cancer
Signs and Symptoms of Thyroid Cancer Paying close attention to signs and symptoms is the best way to diagnose most cases of thyroid cancer early. With this type of cancer, the following signs and symptoms may appear: - A lump (tumor formation) on the neck, sometimes growing rapidly. - Pain in the neck, sometimes spreading to the ear area. - Hoarseness of voice. - Swallowing problems. - Labored breathing. - Cough not associated with an infectious disease. If any of these signs or symptoms appear, you should immediately consult a doctor. Other neck tumors and many non-tumor diseases may cause some of the above symptoms. However, the only way to find out whether these symptoms are related to thyroid cancer is through a medical examination. The sooner the correct diagnosis is made, the sooner treatment can begin and the more effective it can be.
Information about the disease and examination. If signs or symptoms appear that are suspicious for thyroid cancer, you should undergo a full medical examination. Your doctor will ask you about your risk factors, symptoms, and other health concerns. If anyone in your family has had thyroid cancer, especially medullary cancer, or pheochromacytoma, a tumor of the adrenal gland, you should tell your doctor.
During the examination, your doctor will learn more about the signs and symptoms of thyroid cancer and your health status. The doctor will pay special attention to the size and consistency of the thyroid gland and enlarged lymph nodes in the neck and order additional examination.
Test methods: Thyroid scan: During this test, a small amount of radioactive iodine or technetium is injected by mouth or into a vein. The injected radioactive substance accumulates in the thyroid gland and a special camera measures the amount of accumulated substance. Changed areas of the thyroid gland accumulate a smaller amount of radioactive substance compared to surrounding tissues and are called “cold” nodes. Nodes that accumulate more radioactive material are called “hot”.
Most thyroid nodules appear “cold” on scans. Given the fact that both benign and malignant nodules can have “cold” lesions, this test is of little help in diagnosing thyroid cancer. It is performed when the results of a fine-needle biopsy are questionable. If a biopsy confirms thyroid cancer, then a scan helps determine the extent of the tumor process (stage).
After removal of the thyroid gland, a second scan of the gland is performed. Radioactive iodine scanning is often used in patients with papillary and follicular thyroid cancer. This scan is not used for medullary thyroid cancer because the cells of this type of cancer do not accumulate iodine. Scanning the thyroid gland using radioactive iodine gives the most accurate results in patients with high levels of thyroid-stimulating hormone (thyrotropin).
Ultrasound examination: Using this method, the number and size of thyroid nodules are studied. However, with ultrasound, thyroid cancer and benign formations look the same, so this method is often not used.
Computed tomography (CT): This method is not usually used to diagnose thyroid cancer, but is used to determine the stage of the disease.
Magnetic resonance imaging (MRI): The method is very useful in examining cancer patients, as in some cases it allows one to distinguish a benign tumor from a malignant one.
Blood analysis . A blood test cannot diagnose thyroid cancer. However, the determination of thyroid-stimulating hormone in the blood allows one to judge the general condition of the thyroid gland. If medullary thyroid cancer is suspected, calcitonin levels in the blood should be examined. This test can help diagnose medullary thyroid cancer.
Thyroglobulin is a protein produced by the thyroid gland. However, after most of the gland is removed or destroyed with radioactive iodine, thyroglobulin levels should be very low. If this does not happen, then cancer cells are still present. If the level of this protein increases, one can think of tumor recurrence.
Treatment of thyroid cancer Once thyroid cancer is detected, a treatment program is discussed. In this case, both the type of tumor and the stage and general condition of the patient are taken into account.
Treatments for thyroid cancer include surgery, radioiodine treatment, hormone therapy, external radiation, and chemotherapy. It is better to use two or more methods, which allows you to cure the majority of patients with thyroid cancer.
If a cure is not possible for some reason, then it is necessary to remove or destroy as much tumor tissue as possible and prevent the growth, spread or recurrence of cancer for a long period of time. Sometimes only symptomatic treatment is given to reduce the severity of symptoms, such as pain, breathing or swallowing problems. SIGN UP FOR A CONSULTATION by phone +7 (812) 951-7-951
Share link:
Symptoms
| Occurrence (how often a symptom occurs in a given disease) | |
| Frontal headache (migraine) | 70% |
| Double vision (diplopia) | 65% |
| Impaired coordination of movements | 55% |
| General weakness (fatigue, tiredness, weakness of the body) | 50% |
| Weight gain (weight gain, weight gain) | 50% |
| Memory loss (memory impairment, poor memory, memory impairment, forgetfulness) | 50% |
| Daytime sleepiness | 50% |
| Nausea | 50% |
| Vomiting of various types, including indomitable | 40% |
| Hearing loss (hearing impairment, hearing impairment, poor hearing) | 30% |
| Weight loss (emaciation, weight loss, thinness, weight loss, weight loss) | 20% |
| Difficulty speaking (speech disorder, speech disorder, speech problems) | 10% |
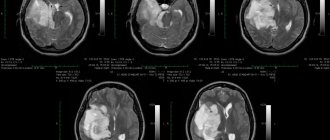
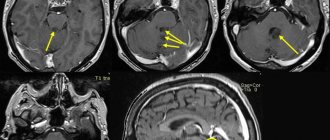
What does a pineal gland cyst look like on CT and MRI?
Computed tomography visualizes a fluid-dense mass with well-defined edges and peripheral calcifications found in 25% of patients. In many cases, there is also a peripheral accumulation of contrast in the cyst in the form of a thin and smooth “rim”. The cyst disrupts the course of the internal veins of the brain, displacing them upward.
Pineal cyst with a typical hyperintense signal on MRI (T2 WI) (marked with a blue arrow). Left: axial tomogram, right – sagittal
The following signs are observed on MRI:
- T1 VI
- Typical iso- or hypointense signal compared to brain parenchyma
- The signal is usually uniform
In 55–60% of cases, the signal is hyperintense compared to the cerebrospinal fluid
- High intensity signal
- High intensity signal that is often not completely suppressed
- There is no diffusion restriction
- Approximately 60% of cysts accumulate contrast