Glioma is a brain tumor that originates from neuroglial cells. Neoplasms are the most common type of malignant pathogenesis of varying degrees of aggressiveness. Symptoms of glioma in adults and children will depend on where it forms. The main diagnostic methods are CT and MRI; the most accurate result is obtained by cytohistological analysis of the selected material (biopsy). The main treatment method for brain glioma is surgical removal of the pathological tumor. Treatment is always comprehensive; in addition to surgery, chemotherapy and radiotherapy are prescribed. Recovery and life expectancy after tumor removal depend on many factors: the adequacy of treatment, the degree of malignancy of the brain tumor, the stage of the disease, the general condition of the patient and many other factors. Benign gliomas have the best prognosis, while grade 3 and 4 gliomas have the worst prognosis. For example, with glioblastoma, life expectancy is usually no more than two years.
Origin of brain gliomas and characteristics
There is still no consensus on which cells give rise to glial tumors. The classical view is based on the fact that gliomas develop from mature glial cells (oligodendrocytes and astrocytes). Recently, they have become more inclined to believe that they are formed in the so-called “malignancy gaps.” This means that brain tumors of this type are formed from immature, slowly proliferating cells that gradually become malignant (degenerate into cancer). How exactly the neoplasm will develop depends on transformations in the genome, for example, astrocytomas (a type of glioma) are formed due to mutations in the TP53 gene,
The share of gliomas in the general population of brain tumors is about 60%. Most often, neoplasms form in the brain and are primary in nature. Brain stem glioma is diagnosed relatively rarely. The color of neoplasia ranges from dark red to soft pink, the shape in most cases resembles a circle or spindle, but can also have irregular outlines. The size depends on the stage of the disease: from a few millimeters to 10-14 cm.
The most common location of the tumor is the area of the chiasmata or cerebral ventricles. Benign glioma, as a rule, does not spread to the bone structures of the skull and does not grow into the membranes of the brain, however, this cannot be excluded. Malignant glioma grows slowly at first, but as carcinogenesis progresses, its growth accelerates. Infiltrative growth is characteristic, i.e. the ability to grow into neighboring tissues, which during diagnosis does not allow defining clear boundaries of the pathogenic focus.
Note. Brain gliomas are not characterized by metastasis, however, they lead to degeneration of neighboring tissues.
Diagnosis of a brain tumor
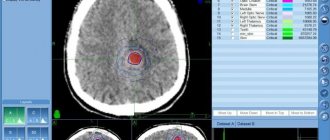
Brain tumors are best detected by MRI. In diagnosing the fourth stage/stage of cancer, studies such as:
- Computed and positron emission tomography. They help detect metastases in other parts of the body. They can also be used to detect the primary focus and distinguish a primary brain tumor from a metastatic one.
- A biopsy is a procedure where a doctor obtains a piece of tumor tissue and sends it to a laboratory for examination. The material can be obtained using a needle under CT or MRI guidance, or during surgery. A biopsy performed with a needle is called stereotactic. In order to perform it, you need to drill a hole in the skull.
Causes and risk factors
Cancer and benign dysplasia can form in the brain at any age, but the likelihood of developing pathology increases as you get older. The overall peak incidence occurs in the seventh decade. The tumor process develops more often in men than in women.
The main causes of brain glioma are the following:
- exposure to ionizing radiation (radiation is the main risk factor);
- genetic prerequisites due to heredity;
- damage by oncogenic viruses;
- head and cervical brain injuries;
- bad habits.
Important. There is no specific prevention against brain cancer. Minimizing risk factors, a healthy lifestyle, quality nutrition, regular exercise and a calm emotional background reduces the likelihood of developing a tumor process.
MRI assistants
Today, the most significant technical breakthrough is observed in the field of preoperative tumor diagnosis. Magnetic resonance imaging (MRI) allows us to characterize the location and volume of the tumor before surgery. Contrast-enhanced MRI is used in three projections and three modes.
MRI spectroscopy is also used to assess metabolism in the tumor and determine the degree of anaplasia (the loss of external characteristics by a cell that can be classified as a certain type), and MRI perfusion is used to determine the volume of blood passing through the tumor.
A very important study for the patient has appeared - functional MRI mapping, which is necessary to determine the proximity of the motor, speech, and visual areas of the brain to the tumor. This is necessary so that the neurosurgeon can calculate how to remove the tumor while causing minimal damage to the patient.
Rice. 2.
Glioma cell culture stained with fluorescent
green
and
red
antibodies for factors important for targeted therapy.
is colored blue
. Photo courtesy of O. I. Gurina from the Federal State Budgetary Institution “National Medical Research Center for Neurosciences named after. V. P. Serbsky"
Classification
Depending on the type of brain cells that degenerated and gave rise to pathogenesis, the following types of tumors are distinguished:
- astrocytomas are the most common type, their share in the general population is about 50%;
- oligodendrogliomas – the share in the general population of tumors of this type is up to 10%;
- Ependymomas are the rarest forms (occurrence less than 7%).
According to the WHO classification (which is generally accepted), neoplasia is ranked depending on the degree of malignancy.
Benign gliomas
These are tumors of the first degree of malignancy, for example, astrocytomas: giant cell, pilocytic, juvenile subependymal. They are benign because they grow slowly, have no signs of cancer, and are easy to treat. The prognosis for life with benign glioma is favorable. After tumor removal, patients live 10 years or longer.
Low grade glioma
Second degree of malignancy. It is also classified as a benign neoplasm, but with a borderline degree of malignancy. The growth of pathological tissue is slow (low-grade), they are well differentiated, as a rule, there is only one sign of cancer (cell atypia). Tumors of this type can degenerate into cancer and easily progress to the third and fourth degree of malignancy. These include diffuse and fibrillary astrocytomas. Treatment is complex: surgery to remove atypical tissues, additionally radio and chemotherapy.
Malignant gliomas
These include gliomas of grade 3 and 4:
- Third degree of malignancy . There are all signs of malignancy, except for tissue necrosis. Tissues lose clear differentiation, tumor growth accelerates (high-grade), the boundaries are unclear, and growth into nearby tissues is typical. The most striking example is anaplastic astrocytoma, which most often develops in middle-aged and older people. Treatment is hampered by the lack of clear boundaries of the tumor; life expectancy depends on how much atypical tissue is removed, as well as the stage of carcinogenesis at the beginning of treatment.
- The most dangerous is the fourth degree of malignancy (glioblastoma). It develops between the ages of 40 and 70 years. In this case, all the signs of malignancy are present, including necrosis. The tumor grows quickly, penetrates other tissues and has no clear boundaries. This significantly complicates therapy. The prognosis is unfavorable.
Neoplasia is divided into two types, depending on growth characteristics:
- Tumors of nodular growth . As a rule, these are benign neoplasms with clear contours. They are characterized by formation anywhere in the brain and the presence of cysts. Examples: pleomorphic xanthoastrocytoma and piloid astrocytoma.
- Diffuse type formations . There are no obvious boundaries, the size can reach significant sizes, neoplasia grows into adjacent brain tissue, which complicates the removal of dysplasia. These are often malignant tumors, such as glioblastoma or anaplastic astrocytoma, or those that can quickly degenerate.
Radiation therapy
Radiation therapy is usually given after surgery and is most often used for high-grade gliomas. But this treatment method can also be used independently.
The type of radiation therapy, dosage regimen and course duration are chosen depending on the type of tumor and some other factors:
- Intensity modulated radiation therapy is a technique that allows you to modulate the radiation dose in three-dimensional space, focusing it as much as possible on the tumor. In this case, neighboring healthy tissues are practically not affected.
- 3D conformal radiation therapy is a method using volumetric planning. The linear accelerator generates radiation that is shaped as close as possible to the outline of the tumor.
- Proton therapy is a technique that uses a stream of positively charged particles - protons - instead of X-rays and gamma rays. They are inhibited in the tumor tissue and emit radiation over a very short distance. Proton therapy units are huge and very expensive, including maintenance, so they are used only in a few medical centers.
- Stereotactic surgery is a radiation therapy method, but at the same time it is a surgical technique. It is used for gliomas with a diameter of no more than 3 cm in the greatest dimension, which are located far enough from critical nerve structures. The device generates many beams that are focused in the right place and literally burn out the tumor without damaging the surrounding tissue. There are different types of machines for stereotactic radiosurgery, some of them use gamma rays (gamma knife), others use x-rays (cyberknife).
Symptoms
Clinical manifestations are divided into general and focal. The latter manifest themselves depending on which part of the brain the pathological formation is formed.
General symptoms
General signs of brain cancer (or a benign tumor) arise due to increased pressure inside the skull, compression of neighboring tissues by the tumor body and the negative influence of its metabolites. Common symptoms include:
- dizziness, headache, discomfort in the head;
- dyspeptic manifestations not related to food intake or poisoning;
- loss of appetite, weight loss;
- blurred vision;
- changing the psycho-emotional behavior habitual for a person;
- memory problems, weakening of mental activity;
- signs of epilepsy.
It's important to understand. That general symptoms are not specific. If they bother you regularly, you need to urgently visit a doctor.
The pathological process in the early stages, as a rule, occurs latently or its signs are weak. Often neoplasms are found by chance, when examining a patient for another disease or for preventive purposes.
Focal symptoms
These are specific signs that arise as a result of damage to the cerebral structures of the central nervous system. The clinical picture depends on the location of the pathological focus:
- Glioma of the optic nerve is formed from cells of its trunk. Tissue growth is slow, accompanied by infiltration, but does not grow into the dura mater. The neoplasm is considered benign; it can form along the entire length of the nerve, but is more often located in the orbital part. Symptoms of optic nerve glioma: first, visual acuity decreases (as the nerve and elements of the eye are damaged), then bulging eyes develop.
- Diffuse glioma of the brainstem is highly malignant. Since diffuse dysplasia is formed in the area where the nerves responsible for the functioning of the limbs are located, when they are damaged, the coordination of the arms and legs is disrupted, up to paresis and paralysis. Clinical signs of diffuse pontine glioma are significant even with small sizes of dysplasia. There are many nerve cords passing through the bridge, so the clinic can be more diverse.
- Glioma of the frontal lobe of the brain is manifested by apathy, mental changes, the person becomes nervous, hot-tempered, and sudden mood changes are characteristic. The later stages of the disease are characterized by the onset of paralysis.
- Glioma of the temporal region causes impaired coordination of movements, memory deteriorates, and diction suffers. In addition, temporal lobe glioma negatively affects the sense of smell.
- Glioma of the cerebellum and cerebellar vermis leads to movement abnormalities. The gait is disturbed, it seems that the person is drunk. This is because it becomes difficult for the patient to maintain balance, his arms and legs do not obey, and maintaining the body in space becomes problematic.
- Glioma of the parietal lobe is accompanied by disturbances in fine motor skills, so a person’s handwriting changes, and over time it becomes difficult to write. Tactile sensations become dull.
- Glioma of the quadrigeminal plate or quadrigeminal plate causes visual disturbances, abnormalities in eye movement, and hearing impairment.
- Glioma of the corpus callosum is accompanied by visual hallucinations (the same ones occur in the presence of a tumor in the occipital lobe), violations of logic, as well as many other signs: changes in sensitivity, muscle weakness, and so on.
- Pontine glioma (diffuse or common) leads to disruption of conduction functions, since the nuclei of the cranial nerves are localized in this area. Therefore, the clinical picture will be quite broad. A violation of sensory perception, movements, and so on is recorded.
- Glioma of the cerebral ventricle leads to an increase in intracranial pressure due to disruption of the outflow of cerebrospinal fluid. Hydrocephalus may develop.
How is treatment chosen, depending on the type of glioma?
For low-grade astrocytomas, treatment usually begins with surgery. These tumors grow strongly into the surrounding healthy tissue, making them very difficult to remove. After surgery, radiation therapy and chemotherapy may be prescribed. The same treatment methods are prescribed in case of relapse.
For high-grade astrocytomas (III and IV), if possible, they try to remove the tumor, after which chemotherapy is prescribed in combination with radiation therapy. Targeted therapy is indicated for some patients. If existing treatments are ineffective, the patient is advised to consider participating in clinical trials.
For oligodendrogliomas, surgery is usually the first option. It helps manage symptoms and increases survival among patients. After surgery, radiation therapy may be prescribed, in some cases in combination with chemotherapy. Radiation therapy and chemotherapy are also sometimes used as neoadjuvant treatment before surgery to shrink the tumor and make it easier to remove. If surgical treatment is not possible, chemotherapy is indicated - alone or in combination with radiation.
For ependymomas, surgical treatment is very effective, since these tumors most often do not invade the surrounding tissue. However, tumor cells often spread into the cerebrospinal fluid. Ependymomas are highly sensitive to radiation.
We will call you back
Message sent!
expect a call, we will contact you shortly
Diagnostics
After an oral conversation and a physical examination (coordination, mental state, work of analyzers and other external signs are studied), the patient is examined using:
- tomography (CT, MRI, PET);
- ultrasound diagnostic methods (echoencephalography);
- EEG (electroencephalogram);
- angiography of cerebral vessels;
- ophthalmological examination;
- scintigraphy and others.
The most reliable method is biopsy (tissue collection is performed when cancer is removed or stereotactic biopsy). Histological analysis of tissue samples gives a complete picture of the type of neoplasm and all its features.
Symptoms of stage 4 brain cancer
Glioblastoma grows very quickly and compresses the brain tissue, causing symptoms:
- Constant headache.
- Convulsive seizures.
- Nausea and vomiting.
- Impaired thinking and cognitive abilities.
- Deterioration of vision, double vision.
- Personality changes, frequent mood swings.
- Restless behavior.
- Loss of consciousness.
At first, these manifestations are not very pronounced, but glioblastoma grows quickly, and they also increase. Symptoms of late-stage brain cancer resemble symptoms of other diseases, so a correct diagnosis can only be made after a thorough examination.
Treatment of brain glioma
Surgical removal of brain glioma is the main method of choice. Treatment is always complex. The results of the operation are supported by the administration of radiotherapy and chemotherapy (before and after the operation). As a rule, surgery to remove gliomas gives a good result only in the case of benign neoplasias that are at the first stage of pathogenesis. At this time, it is possible to completely remove the abnormal tissue.
In other cases this is difficult or impossible to do. Pathological tissues grow into neighboring ones, their boundaries are clearly indistinguishable, so the contour of the tumor cannot be identified, for example, in diffuse types of cancer. Regardless of the method of performing the operation: radical (trepanation or resection of the skull) or minimally invasive (stereotactic techniques and others), their meaning remains the same - it is important to try to remove all the pathological tissue (total removal) or most of it (subtotal).
More often, these tumors are detected at a progressive stage of development, which makes it impossible to perform total removal. In this case, radiotherapy becomes the main method of treatment, for example, this is how diffuse brainstem glioma is treated. Contraindications to surgery may be the presence of other types of cancer, the patient’s poor health or advanced age, the proximity of the cancer to vital structures, the growth of neoplasia in both hemispheres, or a location with difficult access.
Treatment
Like any malignant tumor, brain glioma is treated with three main methods that are used in modern oncology - surgery, radiation therapy (including radiosurgery) and chemotherapy.
The gold standard treatment for brain glioma is surgery. If the tumor is operable, surgery is performed to remove the tumor.
Radiation therapy is performed before and after surgery. For inoperable tumors (if the glioma is localized in a hard-to-reach place), this method is used as a separate method. Today, traditional radiation therapy has been replaced by stereotactic radiosurgery.
Chemotherapy treatment of glioma can be used both preoperatively and postoperatively.
Surgery
The operation to remove malignant glioma is open, involving craniotomy, during which the skull is opened. The main goal of surgery is to remove as much of the tumor as possible while leaving healthy brain tissue intact, thereby preventing neurological damage. A certain localization of gliomas allows the effect of surgical treatment to be achieved up to 98%.
No operation to remove a tumor guarantees a 100% result, since there is always a possibility that cancer cells remain in the brain tissue. However, surgical intervention eliminates compression of surrounding brain tissue and the symptoms of glioma, as well as restores cerebrospinal fluid circulation if intracranial hypertension is present.
The effectiveness of surgical treatment of brain glioma largely depends on the skill and experience of the operating specialists. Treatment of brain tumors at the Oncology Center of the Yusupov Hospital is carried out using high-precision tomographs and neuronavigators, thereby minimizing the likelihood of a relapse of the disease.
Radiation therapy
Radiation therapy may be given before surgery to shrink the tumor before excision, or after surgery to kill any remaining tumor cells.
In addition, this method can be used as an independent method when the tumor is localized in a hard-to-reach place, which prevents its surgical removal. In this case, radiation therapy does not completely destroy the tumor, but can significantly stop its growth.
Traditional radiation therapy is accompanied by a number of undesirable effects: patients experience nausea, decreased appetite, and increased fatigue. At the site of radiation exposure there is a high probability of hair loss and the development of radiation dermatitis. As a rule, side effects of radiation therapy appear 10-14 days after irradiation.
In addition, late complications of radiation exposure are known: patients experience memory impairment to varying degrees, and radiation necrosis may develop (scar tissue forms around the dead tumor tissue).
Radiosurgery
Due to the fact that surgical treatment of brain tumors does not guarantee a complete cure, a relapse of the disease may occur after surgery. Therefore, it is advisable to use additional treatment methods - radiation therapy and chemotherapy. As a rule, relapses are localized at the borders of healthy tissue with the area where the tumor was removed. In such cases, it is recommended to use radiosurgery: cyber knife, gamma knife, Novalis.
Radiosurgery is an innovative method of radiation therapy, the essence of which is to irradiate a glioma with a beam of radiation from different angles, which ensures that radiation reaches the tumor and minimal irradiation of soft tissues.
During the procedure, the position of the patient's head and the location of the tumor are constantly monitored using computed tomography or magnetic resonance imaging, so that the radiation beam is directed exclusively to the malignant neoplasm.
This method is non-invasive, as no incisions are required to perform it. Thanks to this, there is no risk of intraoperative complications and side effects associated with traditional radiation therapy.
In addition, radiosurgery is an absolutely painless method that does not require anesthesia or preparatory measures, and there is no recovery period. The only limitation to radiosurgery is the size of the tumor.
It is important to understand that the effect of radiation therapy occurs gradually, unlike surgery. However, radiosurgery is often the only alternative treatment for inoperable brain gliomas.
Recovery period and life prognosis
The recovery period after removal of a brain glioma will depend on many factors. The most important of them are: the quality of the tumor, its stages, the success of surgical treatment and the general condition of the patient. Generally speaking, the prognosis for life with glioma is unfavorable. With subtotal tumor removal, there is a high risk of relapse, so life expectancy after surgery for brain glioma with partial removal is low. Complete removal is possible at the first stage of a benign tumor. About 80% of patients live longer than five years, provided that the tumor of the first degree of malignancy is completely excised. With relapse of grade 3 or 4 glioma, the prognosis does not exceed two years.
Degrees
There is a WHO classification, according to which gliomas are divided into four grades:
- Grade I – slow-growing benign glioma, which is associated with a long life expectancy;
- Grade II – slowly growing “borderline” brain glioma, which tends to progress to grades III and IV;
- III degree – malignant glioma;
- IV degree – fast-growing glioma of the brain: the life expectancy of patients with this diagnosis is significantly reduced.
1. Tumors of the subcortical ganglia and thalamus opticus
Tumors of the subcortical ganglia and thalamus opticum
are considered one of the most difficult diseases in the field of neurosurgery. This is explained by the severity of the pathological process and the complexity of its treatment. Fortunately, such tumors are quite rare - in about one percent of cases. Gliomas of the subcortical ganglia and thalamus opticus are among the most deeply located supratentorial neoplasms.
Neurosurgeons give cautious forecasts regarding treatment prospects
this pathology, since surgical removal of tumors carries a risk of damage to surrounding brain tissue. In addition, neoplasms of the thalamus are prone to grow into adjacent brain structures - the nerve trunk, great vessels, subcortical nuclei, etc.
A must read! Help with treatment and hospitalization!
Glioma symptoms
The symptoms of a growing glioma directly depend on which part of the brain the tumor occupies. The neoplasm compresses tissues and membranes, which leads to cerebral symptoms:
- Severe headaches that cannot be relieved by taking analgesics and antispasmodics.
- The appearance of heaviness in the eyeballs.
- Nausea resulting from headaches. Patients also complain of periodic vomiting, which also occurs at the peak of an attack.
- Cramps.
If a glioma compresses the cerebrospinal fluid pathways and ventricles of the brain, hydrocephalus develops and intracranial pressure increases. In addition to general cerebral symptoms, glioma also affects the occurrence of focal manifestations of the disease, these are:
- Dizziness.
- Unsteadiness during normal movement.
- Visual impairment.
- Hearing loss or tinnitus.
- Speech function disorder.
- Decreased sensitivity.
- Decreased muscle strength, which causes paresis and paralysis.
In patients with brain glioma, mental changes are also detected, expressed by disorders of all types of memory and thinking, and certain disturbances in behavioral function.
Radiosurgical treatment using the Gamma Knife installation
As a primary treatment, radiotherapy is used to treat benign and malignant gliomas in the initial stages of development. In other options, innovative treatment is used after open surgery and chemotherapy, as well as in cases of recurrent disease.
The radiosurgical unit is a robotic complex equipped with a computerized navigation system and guidance of high-power ionizing beams. The method makes it possible to treat tumors located in places difficult to reach with a surgical scalpel, when the tumor is localized in close proximity to critical areas of the brain. The therapy consists of irradiating the tumor from different angles with minimal consequences for surrounding tissues. In this case, the treatment does not require the use of anesthesia; radiation sessions take place on an outpatient basis without prior preparation of the patient.
Diagnosis of glioma
It begins with asking the patient about complaints and the order of their occurrence. This is followed by a neurological examination, attention is paid to the state of the patient’s mnestic and mental sphere. The following studies can be used in the diagnostic process:
- electroneurography;
- electromyography;
- echoencephalography;
- electroencephalography;
- MRI, CT;
- PAT;
- angiography of cerebral vessels;
- scintigraphy.
If there are complaints of visual disturbances, visometry, perimetry, ophthalmoscopy and convergence studies can be performed. A lumbar puncture is performed to obtain cerebrospinal fluid, which may contain abnormal cells.
The most accurate result in diagnosing a tumor, determining its type and degree of malignancy, can be obtained by stereotactic biopsy or surgery, during which a tissue sample of the tumor node is obtained for further microscopic examination.
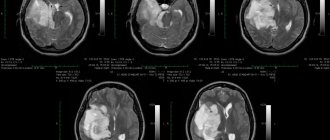
Magnetic resonance imaging (MRI) for glioblastoma
MRI provides a high degree of confidence in the diagnosis of glioblastoma multiforme and is widely used to determine the location and size of brain tumors. In fact, this method has the highest degree of reliability among other radiation methods. Several other processes, mainly masses with a hemorrhagic component, can mimic glioblastoma multiforme on MRI, including brain abscesses and infarcts. In cases of unclear or controversial MRI findings, expert MRI evaluation by specialized radiologists may be helpful.
Standard MRI is limited in its ability to determine the type and extent of malignant transformation of brain tumors, but more advanced MRI protocols, such as perfusion-weighted imaging, can assess this indicator with greater confidence because they can provide more “physiological” information.
What does glioblastoma look like on MRI? As a rule, the lesion on tomograms is an area that has mainly a decreased signal on T1-weighted images and an increased signal on T2-weighted images. Internal cystic areas, areas of signal loss due to large vessels, internal areas of increased signal intensity on T1-weighted images (hemorrhagic lesions), neovascularization, areas of necrosis, extensive peritumoral vasogenic edema, and significant mass effect may be present. An uneven but intense accumulation of gadolinium-based contrast agent can also be detected (the same picture is observed on CT after the administration of iodine-containing contrast), both in the main tumor and in metastatic foci characteristic of MFG. MRI is more sensitive to these changes than CT.
Gliomatosis cerebri appears as a diffuse change in the signal from the white matter, combined with signs of increased intracranial pressure, such as compression of the cerebral ventricles and narrowing of the subarachnoid space.
Gliosarcoma usually presents as a well-circumscribed tumor, with sarcomatous or infiltrating gliomatous elements often resembling meningiomas. Other MRI features are similar to those characteristic of glioblastoma multiforme.
Stages of development
According to the international classification of diseases, the stages of tumor development are assessed according to the degree of danger to the patient’s life. It is customary to divide the disease into four groups or stages of development:
- 1st degree – benign formation with a tendency to slow development. Has the most favorable course of the disease. With timely measures taken, it is possible to extend the patient’s life to 8-10 years. This grade corresponds to congenital benign glioma.
- Grade 2 – the tumor begins to slowly but steadily increase in size. The first signs of degeneration into a malignant formation appear. Signs of deterioration are manifested in a constant increase in neurological and other symptoms.
- Grade 3 – anaplastic glioma. At the third stage, the disease has symptoms characteristic of a malignant neoplasm. Life prognosis does not exceed 2-5 years. There is no metastasis to other areas of the body, but sometimes the spread of cancer to different parts of the hemispheres is observed.
- The prognosis for diffuse brainstem glioma is extremely unfavorable. The patient rarely lives more than 2 years.
- Grade 4 – a large tumor of a malignant nature with a tendency to rapid tumor growth. The prognosis is unfavorable. The patient's life expectancy is up to 1 year. At this stage, inoperable malignant glioma is diagnosed.
Diffuse glioma in young patients is treated radiologically. After a short-term improvement, the disease returns in a more severe form.