Brain tumor – what is it?
A tumor is a voluminous formation, which is a group of atypical cells that are rapidly increasing their population. A tumor in the brain can be either benign or malignant.
All neoplasms of the central nervous system are divided into primary and secondary:
- Primary - those that developed directly in the brain
- Secondary - are metastases of malignant neoplasms of a different location (lungs, kidneys, etc.)
There are a large number of different classifications of tumors of the nervous system. But the histological structure of the neoplasm and its location are of greatest clinical importance.
Based on location, primary tumors are divided into two large groups:
- Brain tumors – account for up to 90% of all central nervous system tumors
- Spinal cord tumors – 10% of central nervous system neoplasms
There are also oncopathologies localized simultaneously in the brain and spinal cord. But their share of the total number of tumors is insignificant - it is a fraction of a percent.
Neoplasms can also be of origin:
- Intracerebral - originate from brain cells
- Extracerebral - comes from blood vessels, nerve sheaths, fragments of embryonic tissue, pituitary gland
Malignant primary brain tumors of intracranial localization have a number of features that distinguish them from cancer of any other location:
- They practically do not metastasize. That is, they do not form daughter tumors in the lymph nodes and other organs.
- The central nervous system is separated from the rest of the body by the blood-brain barrier. Therefore, such tumors usually do not extend beyond the brain.
- Due to the high risk of damage to functionally important areas of the brain, most of these tumors are inoperable.
Due to the above reasons, the classification of tumors according to TNM (tumor size, regional and distant metastases) is practically not used in neuro-oncology. Stages are determined based on the histological type of tumor, and not the extent of the oncological process.
According to WHO, there are 10 histological types of tumors of the central nervous system:
- From neuroepithelial tissue
- From the meninges
- From the nerves
- From hematopoietic tissue
- Germinogenic - from germ cells
- Cysts and tumor formations
- Neoplasms growing into the cranial cavity
- Tumors of the sella turcica (this is a fragment of one of the bones of the skull in which the pituitary gland is located)
- Metastatic tumors
- Unclassified neoplasms
Modern approaches to the treatment of patients with inoperable brain tumors
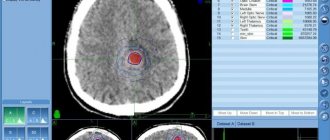
The problem of effective and safe radiation treatment was solved by the introduction into clinical practice of radiosurgical hardware complexes Gamma Knife and CyberKnife, TrueBeam and Triology systems with innovative linear accelerators, tomotherapy units with multi-leaf collimators, as well as the opening of proton therapy centers.
The choice of the most appropriate method, device and treatment regimen is determined taking into account the characteristics of the technology, tumor and patient.
For example:
- Proton therapy can successfully treat children and adolescents with inoperable brain tumors. This not only minimizes the risk of side effects immediately after the procedure, but also preserves the possibility of further normal development of the child’s central nervous system in the long term.
- The new generation of Gamma Knife devices, such as the latest model of the device produced by the Swedish company Elekta, allows for optimal distribution of the radiation dose in tumor tissues and increases the dose if it is necessary to enhance the destructive effect. In this case, hard irradiation does not affect adjacent healthy tissue, and the use of a stereotactic frame is not required, which increases the comfort of the procedure, expands its capabilities and reduces the likelihood of complications.
- Using CyberKnife, specialists are able to irradiate larger tumors than with Gamma Knife, as well as irregularly shaped tumors.
- True-Beam and Triology installations make it possible to destroy tumors larger than 6 cm.
Using conformal radiation therapy using the TrueBeam STx installation, you can quickly and effectively destroy inoperable tumors of large size and complex shape
- When using the tomotherapy method, radiotherapists can specifically irradiate several tumor nodes at once without harming healthy brain tissue. No other technology provides such capabilities.
Modern drugs and treatment regimens are gentle. This makes it possible to minimize the likelihood and severity of chemotherapy side effects. In addition, drugs have recently been synthesized that can successfully cross the blood-brain barrier.
- In recent years, the possibility of minimally invasive laser ablation of brain tumors has become possible.
The technology used offers hope to a significant number of patients with deep/hard-to-reach brain tumors who were denied surgical treatment because it carried an unreasonably high risk of damaging vital parts of the brain.
It also reduces the risk of infection, does not require a long hospital stay (1 day compared to 5-10 days after open brain surgery), reduces recovery time, requires virtually no hair removal, and leaves little to no scarring.
Professor K. Ashkan, a neurosurgeon at the Harley Street Clinic, one of the most respected cancer clinics in the UK, emphasized that: “Visualase technology combines laser surgery and robotics using the keyhole principle. The precision of laser ablation is ensured by real-time MRI control and the ROSA robotic control system. A flexible catheter with a diameter of 1.65 mm and a shallow bone anchor provide wide surgical access. All this makes it possible to safely treat brain tumors in places that were previously considered inaccessible. The minimally invasive nature of the intervention allows for rapid recovery from therapy with a minimum length of hospital stay. "Visualase will benefit patients with a range of neurological and neurosurgical disorders, especially epilepsy and brain tumors."
Thus, today there is a chance to enter remission while maintaining quality of life even in the most difficult situations - including in patients previously considered hopeless.
Gliomas
Gliomas are tumors of neuroepithelial tissue. They make up more than half of all tumors of the central nervous system. This type of brain tumor is most often the result of genetic mutations. These include glioblastomas, astrocytomas, and ependymomas. Some develop for a very long time - years. Others progress rapidly and lead to the death of the patient within a few months.
Gliomas have 4 degrees of malignancy. Typically, grade 1-2 tumors are called benign, grade 3-4 tumors are called malignant. The latter include glioblastoma and anaplastic astrocytoma, the most common neuroepithelial tumors of the central nervous system. They account for up to 80% of all neoplasms of this type.
Tumors from the meninges
Neoplasms from the meninges account for about 20% of primary CNS tumors. 95% of cases of cancer of this type are meningiomas. The remaining 5% are fibrous histiocytomas, hemangiopericytomas, melanomas, diffuse sarcomatosis and others.
Some risk factors for tumors from the meninges have been established. Here's what can cause a brain tumor:
- Head injuries
- Ionizing radiation (including radiation therapy)
- Eating Nitrites
Genetic defects in chromosome 22 have been identified, due to which a brain tumor can develop. The cause is a mutation at the 22q12.3-qter locus.
According to malignancy, meningiomas are divided into 3 groups:
- Grade 1 - includes 9 histological types, the most common of which are meningoepithelial (60% of cases), transitional or mixed (25%) and fibrous (12%)
- Grade 2 – these are atypical meningiomas, which are marked by rapid cell division and rapid growth
- Grade 3 – anaplastic meningiomas (old name – meningosarcoma)
Rarely, multiple brain tumors occur. The reasons for their occurrence are not known. They make up about 2% of all diagnosed meningiomas. Such neoplasms are characterized by a favorable clinical course. In 90% of cases, a person lives a full life with them, without any symptoms. Only 10% of cases require surgical removal of tumors.
Send a request for treatment
Pituitary tumors
Up to 10% of all intracranial neoplasms are pituitary tumors. They are almost always benign. They usually develop from cells of the adenohypophysis (the anterior lobe of this gland). Such neoplasms are called adenomas, and if they have a diameter of less than 1 cm - microadenomas. What causes a brain tumor of the corresponding localization has not yet been established.
Although some risk factors are known:
- Brain infections
- Traumatic brain injuries
- Toxin poisoning
- Use of oral contraceptives
- Obesity
The causes of a tumor in the brain that grows from pituitary gland cells may be due to gene mutation. Hereditary predisposition is of no small importance. At what age can a brain tumor of adenohypophyseal origin develop? This is one of the “youngest” tumors. It occurs in everyone, including children. The peak incidence occurs in working age - from 30 to 50 years.
Most pituitary adenomas are not accompanied by severe symptoms, so their detection rate is low. Treatment is usually carried out conservatively (normalizing the level of hormones in the blood). When it stops working, surgery is used.
Germ cell tumors
Germ cell tumors in the brain develop from embryonic tissue. These neoplasms include germinoma, choriocarcinoma, yolk sac tumor, and embryonal carcinoma. They are located in the area of the epiphysis. The most common is germinoma. It accounts for up to 0.5% of all brain tumors in representatives of the European race, and up to 3% in Asians. The reasons why this brain tumor occurs more often in the Asian population are not known. It is diagnosed more often in boys. The tumor is malignant - it metastasizes through the cerebrospinal fluid (the fluid that washes the brain).
Metastatic brain tumors
About 20% of the structure of CNS neoplasms are metastatic brain tumors. The causes of these diseases are obvious: the spread of metastases from other parts of the body. It is believed that their actual prevalence is even higher. After all, cancer patients with stage 4 cancer are often not examined too carefully due to the inappropriateness of in-depth diagnostics. Even if there is a suspicion that they have a brain tumor due to cancer of another location, such patients are no longer referred to neurosurgeons.
What can cause such a brain tumor? Here are the most common reasons:
- Lung cancer – 40% of cases of metastatic damage to the central nervous system
- Breast cancer – 10%
- Kidney – 7%
- Stomach or intestines – 6%
- Melanomas - on average 5%
Prognosis for renal secondary tumors
The spread of cancer cells and their subsequent localization inside the kidneys directly determines life expectancy (subject to proper treatment and elimination of metastases). The chances that atypical cellular components will settle in the kidneys are unusually high, because they are transported along with the blood mass and lymph through this organ. Often, such localization is characteristic of primary cancerous lesions of the larynx, pharynx, and intestines.
Life expectancy depends on the stage at which the underlying cancer pathology was discovered. However, the forecasts are still often pessimistic, because at the first stages of metastatic involvement of the kidneys, their functional qualities are not impaired in any way. For this reason, metastases are difficult to detect (only a complete examination can identify them).
After diagnosis, the oncologist develops treatment tactics. To effectively influence renal metastases, you need to combine several techniques. As a rule, surgery and therapeutic methods are combined. The effectiveness of radiation treatment and “chemotherapy” for renal metastases is very low. Often, only removal of pathogenic tissue helps. Statistics indicate that survival rate with renal metastases is higher than with metastases affecting other organs. About 40% of patients reach the 5-year time barrier, although such a result requires complex therapy and nephrectomy.
Tumors of childhood
Even children can get a brain tumor. Among childhood cancers, brain tumors account for about 20%. This is second only to leukemia. More often they are observed in children of the first year of life. Teratomas are found mainly in children. In older children, benign astrocytomas (more than 30%), primitive neuroectodermal tumors (medulloblastoma, pineoblastoma - 20%) and ependymomas (15% of cases among children over 1 year of age) predominate.
At present, it is not known for certain how brain tumors form in children. It has been established that they develop more often in boys than in girls. The reasons why brain tumors are more common in male children have not been established.
How can you get a brain tumor?
Patients often ask their doctor how they can get a brain tumor. They suggest that knowing the causes will help prevent the disease. Unfortunately, it is not. For many types of cancer, the underlying etiological factors have indeed been established. For example, it is well known that lung cancer occurs mainly due to smoking, cervical cancer is caused by human papillomavirus infection, and liver cancer is caused by viral hepatitis C. But what causes a brain tumor is still not known. Despite numerous clinical studies, scientists have not been able to establish the causes of brain tumors.
However, some risk factors have been identified:
Radiation . There are many ways you can get a brain tumor due to radiation. Most often this is radiation therapy for cancer or occupational hazards (radiologists, nuclear industry workers). In children, in the old days, the cause of brain tumors was radiotherapy used for fungal infections of the scalp.
The connection is not always clearly visible. After all, the first symptoms appear only 10-15 years after irradiation. But a retrospective analysis of medical records shows what can cause a brain tumor. Anamnesis data demonstrate that neoplasms of the central nervous system are more often observed among individuals exposed to radiation exposure.
Does this mean that a brain tumor occurs from radiography, fluorography or computed tomography? After all, these methods are based on the effects of ionizing radiation. No, no such connection has been established. Even decades ago, when the devices were much less advanced and gave tens of times more radiation load, there was no reason to believe that a brain tumor could occur as a result of the diagnostic procedures performed. Today, the devices used are so precise and perfect that the radiation is minimal, without damaging cells or causing mutations.
Heredity . Some genetic abnormalities have been identified that may cause a brain tumor. These include neurofibromatosis type 1, type 2, tuberous sclerosis, Hypeel-Lindau disease, Li-Fraumeni syndrome. There are other genetic causes of brain tumors, but they are much rarer.
Immunity . One of the types of neoplasms of intracranial localization is lymphoma. This brain tumor can occur due to decreased immunity. This is caused by AIDS, treatment after organ transplantation (immunosuppressive therapy), long-term use of immunosuppressants and glucocorticoids for dermatological diseases or systemic connective tissue lesions.
There are also several mythical reasons worth noting. Many people are afraid of them, but these fears are false.
So, here's what a brain tumor can't cause:
- Using a mobile phone – contrary to popular belief, it does not emit ionizing radiation
- Playing soccer (soccer players often head the ball)
- Exposure to electromagnetic fields
- Hair dye
- Stress and bad habits
We also note several controversial reasons why a brain tumor can occur. These risk factors are suspected but not yet definitively proven.
Among them:
- Aspartame (sweetener for diabetics)
- Exposure to vinyl chloride (occupational hazards in plastics production)
- Viral infections
- Exposure to petroleum products
Thus, scientists do not yet know exactly what causes a brain tumor. Therefore, the only thing you can do to prevent this disease is not to expose yourself to massive ionizing radiation and, if possible, maintain a good immune system.
Formations in the spine
Metastatic lesions of the spinal column pose a direct threat to life. Almost always, vertebral metastases progress multiple times. If such a lesion is not detected in a timely manner, a person dies within a few months. The main symptom of this disease is pain in the spinal column, which gets worse at night. Then all sorts of neuralgic abnormalities come to the fore. In the absence of therapeutic measures, numbness of the arms and legs and disruption of organ function are possible.
To make predictions, additional diagnostic procedures are carried out. Treatment is required. With timely care, more than 80% of patients survive to the 5-year mark.
Meningeal brain tumor - prognosis
The survival rate for meningiomas is high. The clinical course of the disease is favorable. Usually these are neoplasms of 1st degree of malignancy. If there are no symptoms of pathology, an observation strategy is used. Surgery may not be necessary because most of these brain tumors have a good prognosis.
The first thing patients are interested in is how long do they live with a brain tumor of meningeal origin? This depends on a number of factors. First of all, it depends on the degree of malignancy, as well as the treatment performed.
If the brain tumor was completely removed during surgery, how long people live depends solely on their age and health status, because meningioma does not recur with a 95% probability. Only 5% of patients experience recurrences within 15 years after surgery.
But sometimes the neoplasm is localized in functionally active structures of the central nervous system. In such cases, complete removal is not possible. However, even if it was partially removed, the risk of recurrence within 15 years is only 50%. In the remaining 50% of cases, the tumor remains the same size - it does not grow. If growth of meningioma is observed, it responds well to treatment with radiation therapy. Even for malignant meningioma, radiation helps control tumor growth for at least 5 years.
The age of the patient is also important. Below you can see data on how long people live with a meningeal brain tumor, depending on age.
The percentage of five-year survival is indicated - that is, the number of people who will live for 5 or more years after diagnosis:
- Up to 45 years – 87%
- Up to 55 years – 77%
- From 55 to 65 years – 71%
In most cases, after 5 years the tumor no longer recurs if it was completely removed during surgery.
Prognosis and survival
Brain cancer is a fairly serious problem. The prognosis depends on the stage of the disease - the earlier it is diagnosed, the greater the chances of a positive result.
- At the first stage, when the formation is not malignant, is diagnosed on time and develops slowly, treatment allows us to give the most optimistic prognosis.
- In the second case, when neurological symptoms appear, the prognosis is not so favorable.
- When diagnosing the third and fourth stages, especially in cases where the tumor is growing rapidly and can no longer be treated surgically, life expectancy is greatly reduced.
Of all types of tumors, astrocytoma has a more benign course and, accordingly, a favorable prognosis. But this depends on age and the radical surgery performed correctly. The optimistic prognosis for 5-year survival under favorable conditions is 80%. Sometimes an astrocytoma develops into a tumor with malignant growth, which requires additional types of treatment. Therefore, when diagnosing astrocytoma, it is necessary to be under the supervision of an oncologist.
Neuroepithelial brain tumor – how long to live?
If you have been diagnosed with a neuroepithelial brain tumor, how long to live cannot be definitely said without establishing its histological type. It is the structure of the neoplasm that determines how long a brain tumor takes to develop.
Based on this parameter, there are 4 degrees of malignancy of neuroepithelial neoplasms of the central nervous system:
- Grade 1 – pilocytic astrocytoma
- Grade 2 – protoplasmic, pleomorphic, hemistotic, fibrillary astrocytoma, xanthoastrocytoma and ependymoma
- Grade 3 – anaplastic astrocytoma
- Grade 4 – glioblastoma
Grade 1 and 2 neuroepithelial brain tumors are considered low grade. They have a more favorable prognosis. Grades 3 and 4 are neoplasms of high malignancy or simply malignant. The worst prognosis is characterized by a grade 4 brain tumor.
How long do people live with glioblastoma ? Unfortunately, this tumor has a worse prognosis. It develops very quickly and is manifested by necrosis (death) of parts of the brain. From the moment the tumor appears to the first symptoms, sometimes not even months, but weeks pass. The average life expectancy for patients under 40 years of age is no more than one and a half years, and for patients over 40 years of age – less than 1 year.
Five-year survival rate in developed countries, depending on age:
- Up to 45 years old – 19%
- From 45 to 55 years – 8%
- From 55 to 65 years – 5%
Patients do not even always undergo surgery, since they die from a grade 4 brain tumor quite quickly. Often only radiation and chemotherapy are used. But these methods do not significantly prolong the patient’s life. Unfortunately, glioblastoma is the most common glioma (neuroectodermal tumor). It makes up about 50% of the structure of these neoplasms.
Anaplastic astrocytoma is another malignant brain tumor. How long do people live with this disease?
Average life expectancy, depending on the patient’s age at the time of diagnosis:
- Up to 40 years – about 3 years
- From 40 to 60 years – on average 2 years
- After 60 years – less than 1 year
Five-year survival rate, depending on age:
- Up to 45 years old – 54%
- From 45 to 55 years – 32%
- From 55 to 65 years old – 14%
The pathology is characterized by infiltrative growth. That is, the tumor penetrates the brain tissue, rather than displacing it. Anaplastic astrocytoma is the second most common neuroectodermal tumor after glioblastoma. In the structure of these neoplasms it makes up about 30%.
The next most common tumor of the central nervous system from neuroectodermal tissue is oligodendroglioma . It accounts for about 5% of all gliomas. The average life expectancy of patients in developing countries, including the CIS, is 6 years. In developed countries (Germany, USA) the indicators are much better.
The five-year survival rate, depending on the age of the patient at the time of diagnosis, is:
- Up to 45 years – 88%
- From 45 to 55 years – 81%
- From 55 to 65 years – 68%
Unfortunately, sometimes oligodendroglioma becomes malignant. In this case, it acquires grade 3 malignancy, and the prognosis worsens. It is not known for certain what causes the brain tumor anaplastic oligodendroglioma. However, the life expectancy of patients is reduced.
Five-year survival rates for this type of neoplasm in developed countries:
- Up to 45 years – 71%
- From 45 to 55 years – 61%
- From 55 to 65 years – 46%
Ependymomas make up about 3% of gliomas. They are more common in children than in adults. Most often these are benign tumors. Anaplastic ependymomas (grade 3 malignancy) are rare. There is no data on what causes this brain tumor in children. Survival rates vary significantly between countries. In the CIS, the five-year survival rate for children over 3 years of age is about 50%, for adults – 70%. In developed countries, the statistics are much better due to better treatment.
Five-year survival rate for patients with ependymoma in countries with well-developed medicine:
- Children's age – 75%
- Patients from 20 to 45 years old – 92%
- From 45 to 55 years – 89%
- From 55 to 65 years – 86%.
Survival of patients with breast carcinoma who develop brain metastases is closely related to the subtype of carcinoma. The same applies to the location of metastases.
HAMBURG. Approximately 30% of patients with metastatic breast cancer develop metastases to the brain despite systemic therapy. After lung cancer, breast cancer ranks second among malignant neoplasms, which in most cases metastasize to the brain. In general, malignant tumors are more often located in the brain than primary tumors.
The increasing incidence of brain metastases in patients with breast cancer is likely due in part to the fact that it is now possible to provide better control of the disease outside the skull. This is also facilitated by improving the quality of imaging diagnostics. However, at the same time, the increasing incidence of brain metastases also indicates the inability of the current treatment regimen to prevent tumor spread to the brain.
In order to raise awareness of the clinically important group of patients whose breast cancer has metastasized to the brain, leading breast centers in Germany have united under the auspices of the German Breast Group to jointly conduct the “Brain Metastases in Breast Cancer Network Germany” (BMBC) study. Recently, a research group led by Isabelle Witzel from the University Hospital Hamburg-Eppendorf published in the European Journal of Cancer (2018; online August 9) an analysis of data from 1,712 breast cancer patients with brain metastases from 2000 to 2021 gg.
The average age of women was 56 years (22-90). 48% of women were diagnosed with HER2-positive tumors, 21% with triple-negative breast cancer, and 31% with luminal breast cancer (hormone receptor positive, HER2 negative). The proportion of HER2-positive brain metastases decreased during the study period; in 2000-2009 it was 51%, and in 2010-2015. - 44%. The number of cases of luminal types of cancer, on the contrary, increased proportionally from 28% to 34%.
Metastases were localized in the anterior cranial fossa (31%), in the posterior cranial fossa (23%), or in both cranial fossae. Leptomeningeal metastases were diagnosed in 9% of patients. 54% of metastases in the posterior fossa were HER2-positive, 60% of leptomeningeal metastases were of the luminal type.
92% of patients had at least one attempt at local therapy. 28% of patients underwent surgery, and 94% of patients received radiation therapy after surgery. 64% of patients received radiation therapy, which included stereotactic treatment (7%), whole-brain irradiation (89%), or both.
After diagnosis of brain metastases, the average life expectancy of patients remained 7.4 months. 38% survived the first year. The average survival time for patients with HER2-positive tumors was a maximum of 11.6 months, compared with 5.9 months for patients with luminal tumors and 4.6 months for patients with triple-negative metastases. With anti-HER2 therapy, the average life expectancy of patients with HER2-positive tumors was 17.1 months; without such treatment, patients lived an average of 7.2 months.
“The prognosis for patients whose breast carcinoma has metastasized to the brain depends largely on the tumor subtype,” summarizes Witzel and her colleagues. The results highlight the urgent need to improve treatment and prevention strategies for such metastases in women with breast cancer.
The average life expectancy for breast cancer patients with HER2-positive brain metastases was 11.6 months. With luminar type of tumors, the life expectancy of patients was 5.9 months, in the presence of triple-negative metastases - 4.6 months.
Contact us
The Center for Diagnosis and Treatment of Breast Cancer at the City Clinical Hospital of Solingen is one of the most famous and modern not only in Germany, but in Europe. If you have any doubts about your health, please contact our specialists for advice: Email: [email protected] Tel.: +49 212 5476913 Viber | WhatsApp: +49 173-2034066 | +49 177-5404270 For your convenience, please save the phone number in your phone book and call or write to us for free on WhatsApp, Viber or Telegram. Applications made on weekends or holidays will be processed on the first business day. In urgent cases, request processing is carried out on weekends and holidays.
How long do they live with a brain tumor from fetal tissue?
Germ cell tumors are malignant. They occur in children. They are characterized by metastases. The most common tumor is germinoma. It is also the most favorable. In the vast majority of patients, even without the use of surgical methods, this malignant brain tumor is cured. How long do they live after treatment? Life expectancy is potentially the same as that of a person who has never suffered from this pathology. To cure the disease, radiation therapy and sometimes chemotherapy (in children under 4 years of age) are sufficient. The younger the age, the better the prognosis. Unfortunately, the prognosis for other types of germ cell tumors is much worse. They are very rare. But patient survival is extremely low. These are inoperable brain tumors. How long do patients live? Only 5% of patients will live more than 2 years after diagnosis. Radiation therapy and chemotherapy are used for treatment, since surgical treatment does not improve the prognosis. Only palliative operations are performed. For example, shunting surgical interventions for blockage of the cerebral aqueduct.
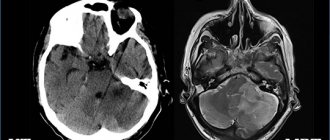
Diagnostics
Early diagnosis of brain cancer is theoretically possible, but unlikely. Screening (preventive examination of clinically healthy individuals) is carried out only for patients from risk groups who have a family history or genetic syndromes. The tumor can be detected using a CT scan or MRI of the brain.
Most patients see a doctor after the first symptoms of brain cancer appear. The main diagnostic method is MRI. It is this technique that allows you to obtain a detailed image of all brain structures, identify even small tumors, and suggest their histological type even before conducting a histological examination.
Metastatic brain tumor – how long to live?
In many cases, cancer is detected after metastases have appeared in the central nervous system. How long people live with a metastatic brain tumor depends on the treatment provided. In the natural course of the disease, the average life expectancy of patients is about 3 months. With surgical treatment or radiation therapy, it can reach 2 years or more. Life expectancy also depends on the histological type of cancer, location and number of metastases. In approximately 50% of cases they are multiple, which worsens the prognosis.
Send a request for treatment
Brain cancer: symptoms
Manifestations of the disease depend on the location and stage at which the process is located. Usually this:
- headache;
- nausea and vomiting;
- epileptic seizures;
- deteriorating memory;
- balance is disturbed;
- dizziness occurs;
- unsteadiness when walking;
- difficulty speaking;
- loss of sensitivity or paralysis of a part of the body;
- deteriorating vision;
- behavior changes.
Symptoms of brain cancer increase as the tumor progresses, and new ones appear. If you notice changes in your health or the appearance of unusual symptoms, you should consult a specialist and undergo an examination as soon as possible.
Where to go if you have brain cancer?
The diagnosis and treatment of brain cancer and astrocytoma are the most successful in Germany and other developed countries, which is confirmed by patient survival statistics. If you want to use the services of German doctors, please contact ]Booking Health[/anchor]. We organize treatment abroad.
Our advantages:
- A team of doctors who understand modern methods of treating various diseases will select the best clinic for the treatment of brain cancer for you.
- Thanks to direct contracts with the best medical institutions in Germany, you can save up to 70% of the cost of the treatment program. In addition, the waiting time for a doctor’s appointment will be reduced.
- The initially agreed cost of treatment is guaranteed not to change. Even if complications arise and additional therapeutic measures are required, all unforeseen expenses will be covered by insurance.
- A full package of services: we will completely organize the entire treatment process in Germany, provide an interpreter, and provide transfer from the airport to the clinic.
- Absolute transparency of financial relationships: you can always find out what services you paid for and in what volume. Unused funds after treatment will be returned.
To take advantage of all the benefits of German medicine, leave a request on our website. After processing it, we will contact you and you will be able to receive comprehensive advice on the treatment of brain cancer abroad.
Treatment
The main methods of treating brain cancer:
- classical neurosurgical operation - involves craniotomy and tumor removal;
- endoscopic surgery - involves inserting instruments and a camera through small holes in the skull (performed for pituitary tumors, which are removed through the nose, as well as superficially located tumors of some parts of the cerebral hemispheres);
- laser ablation of tumors under MRI control;
- radiosurgical methods - destruction of small tumors with precisely directed beams of radiation;
- radiation therapy;
- chemotherapy;
- targeted therapy.
Our expert in this field:
Sergeev Pyotr Sergeevich
Oncologist, surgeon, chemotherapist, Ph.D. Member of the international society of surgical oncologists EESG
Call the doctor Reviews about the doctor