Cervicocranialgia; Barre-Lieu syndrome; spinal nerve syndrome; Cervical migraine, vertebral artery syndrome; Neuritis of the sympathetic vertebral nerve - under such names can be found in foreign and domestic medical literature - Posterior cervical sympathetic syndrome.
The syndrome described above is generally considered to be a functional stage of vertebral artery syndrome. Vertebral artery syndrome refers to cerebrovascular diseases that lead to vascular disorders of cerebral circulation. Brain strokes are the main cause of disability and mortality among the adult population of planet Earth!! This problem, which is extremely unfavorable in epidemiological terms, also exists in Ukraine.
- The reasons are impaired blood circulation in the vertebral arteries, compression of blood vessels in the cervical spine.
Clinical picture
Headache in the cervico-occipital region, radiating to the parietal, temporal, fronto-orbital and ear regions, more often on one side. The headache is throbbing, aching, burning in nature and is provoked by head movements. Often, cervicocranialgia is combined with short-term vestibulo-cochlear disorders (balance disorders), sometimes with transient visual (blurred vision, darkening of the eyes). Physical and mental performance decreases sharply.
Vertebral artery syndrome. Pain, a feeling of numbness, a “crawling sensation” in the cervical-occipital region with irradiation to the anterior parts of the head, parietal, temporal, and postauricular regions. There is a sensation of a foreign body in the eye on the affected side, dizziness, nausea (or vomiting), congestion in the ear, tinnitus. There may be sensations of falling through, surrounding objects falling on the patient, a transient decrease in visual acuity, the patient falling without loss of consciousness - falls of the dropp attack type. Unsteadiness when walking. Possible increase in body temperature. General weakness, increased irritability, mood instability, feeling of heaviness in the head, sleep disturbances, memory problems.
Barré-Lieu syndrome (cervical migraine)
Signs
Barré-Lieu syndrome is characterized by a constant dull headache, sometimes throbbing.
It is localized in the cervical-occipital region and can spread forward to half of the head (which is why this condition is called cervical migraine). Pain often occurs during prolonged forced head position, for example, while working at a computer or in a movie theater. It intensifies with fast walking, shaking in transport, going up and down stairs. This pain can last from several minutes to several hours. Sometimes headaches are accompanied by paresthesia (impaired sensitivity, numbness), “tightening” of the head, “bulging” of the eyes, and burning or cold sensations. Also, with cervical migraine, patients complain of pain and tinnitus, nausea, dizziness, pain in the eye area, temporary decreased vision, the appearance of fog and spots before the eyes, and fatigue. There may also be sweating, chills, and hot flashes.
The gesture of “removing the helmet” is typical for those suffering from Barré-Lieu syndrome - when the patient shows exactly where his head hurts, he runs his half-bent hand over his head from the back of his head to his forehead. Sometimes patients complain of a feeling of a lump in the throat. In the later stages of the disease, irritability, sleep disturbances, memory loss, and fainting are possible.
If you notice these symptoms, contact your rheumatologist.
Description
This disease was first described by the French neurologist Barre in 1925 and the Chinese doctor Lieu in 1929.
Cervical migraine develops due to damage to the I, II and III cervical vertebrae, as a result of which the roots of the spinal nerves that intertwine the vertebral artery are compressed. The artery is also compressed. The result is circulatory failure, swelling of the nerves and stagnation of venous blood. Moreover, circulatory failure occurs not only at the site of damage to the vertebrae, but also in some structures of the brain. Such changes in the vertebrae can occur due to osteochondrosis, spondylosis, spinal trauma, or its tumor. The disease can also be caused by cervical lymphadenitis (inflammation of the lymph nodes), cervical arachnoiditis (inflammation of the arachnoid membrane of the spinal cord), stenosis (compression) of the vertebral and basilar arteries.
Often during attacks, cervical migraine sufferers are unable to work.
Diagnostics
Diagnosing Barré-Lieu syndrome is quite difficult, as it has many manifestations. To correctly make a diagnosis, you need to carefully collect anamnesis, conduct magnetic resonance imaging or spiral computed tomography of the cervical spine, and duplex scanning of the vertebral artery.
It is also necessary to carry out a differential diagnosis with Meniere's syndrome. In contrast, with cervical migraine there are no vestibular disorders (the sense of balance is not impaired).
Treatment
In case of acute pain syndrome, bed rest is prescribed for 3 days, then semi-bed rest for 3-5 days. In bed, it is better to lie on your back, with a small low pillow. It is recommended to place a bag of heated sand under your neck to provide dry warmth. In addition, this pouch will support the spine in a comfortable position. It is recommended to fix the cervical spine with a soft collar.
One of the main methods of treating cervical migraine is physical therapy. Electrophoresis with a solution of aminophylline or analgin is prescribed; phonophoresis with hydrocortisone and magnetic therapy are prescribed on the back of the neck and shoulder girdle. If for some reason it is impossible to carry out physical therapy, the doctor prescribes mustard plasters, dimexide applications with non-steroidal anti-inflammatory drugs, anti-inflammatory and warming ointments.
To correct vascular disorders, drugs that improve cerebral circulation are prescribed.
After the pain has decreased, physical therapy is prescribed. The complexity of the exercises depends on the patient’s age, the severity of osteochondrosis, and concomitant diseases. But rotational movements of the head and throwing the head back are contraindicated for everyone. Exercises are done to strengthen the muscles of the neck and trapezius muscles. To reduce decompression of the nerve roots, the neck is extended in sitting, standing and lying positions. True, a professional should stretch the neck and this must be done very carefully, as otherwise you can provoke a headache and dizziness. Pull-ups are contraindicated for those suffering from hypertension and cerebral atherosclerosis.
In the remission phase, sanatorium-resort treatment is indicated. The health of those suffering from Barre-Lieu syndrome is favorably influenced by radon, pearl and hydrogen sulfide baths, mud, and massage.
Prevention
In order to prevent the development of Barré-Lieu syndrome, you need to monitor the condition of your spine, because it is because of a violation of its integrity that cervical migraine occurs. That is, you need to strengthen your back muscles, monitor your posture, avoid spinal injuries and eat right. Food should not be oversalted, it should have a balanced content of proteins, fats and carbohydrates, since all these components are important for the health of the vertebrae and intervertebral discs.
© Dr. Peter
Peripheral neurovascular syndromes. Illness of young people
S.A. Klyushnikov Candidate of Medical Sciences, State Research Institute of Neurology, Russian Academy of Medical Sciences
Peripheral neurovascular syndromes (NVS) are a combined lesion of neurovascular formations of the neck, shoulder girdle, trunk and limbs. These diseases are widespread among the population and can cause permanent disability in young people. The development of symptoms, as a rule, is caused by long-term pathological effects of various external and internal factors on the neurovascular bundles with disruption of the conduction of nerve impulses in the walls of blood vessels and directly in the tissues.
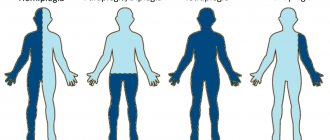
The clinical picture of SVC is characterized by a combination of pain, muscular-spastic and vegetative-vascular disorders, often with the addition of edematous-dystrophic tissue changes. Clinical signs of NWS are conventionally divided into: • local - muscle soreness and tension, pain points in typical places, tissue swelling • neurological - muscle atrophy, contractures, etc. • vascular – changes in temperature and skin color (cyanosis), changes in blood pressure and pulse on one limb
Well-known forms of NVC are, for example, tunnel neuropathies, often also called “trap neuropathies.” This is the infringement of peripheral nerves and vessels by tendons and ligaments in anatomical narrowings (tunnels) through which neurovascular bundles normally pass - in hard bone canals, openings in ligaments, etc. Currently, the role of congenital narrowing of the bone and connective tissue canals in the development of this form of congenital fibrosis has been established. Compression is also possible with a normal diameter of the canals in the case of an increase in the diameter of the nerve due to edema. A classic example is the development of neuropathy (“paralysis”) of the facial nerve, when, under the influence of some external factor (for example, hypothermia), microcirculation in the area of the facial nerve is disrupted, swelling of the nerve trunk develops, and the nerve seems to compress itself in the bone canal . Some of the most common forms of neurovascular syndromes are:
— Vertebral artery and vertebral nerve syndrome (synonyms: posterior cervical sympathetic syndrome, “cervical migraine”, etc.). The reason is irritation of the spinal nerve due to pathology of the cervical segments of the spine, resulting in the development of a reflex spasm of the vertebral artery. Characterized by headaches, dizziness, a combination of vestibular disorders with pain points on the neck in the projection of the entrance of the vertebral artery into the spinal canal, and various autonomic-sensitive disorders in the head area.
— Scalenus syndrome (anterior scalene muscle syndrome). It consists of compression of the subclavian artery and brachial plexus between the anterior and middle scalene muscles in the neck. As a result, a decrease in blood pressure in one arm and a decrease in the filling and tension of the pulse develop, cyanosis and autonomic disturbances appear in the arm below the point of compression, pain and numbness in the shoulder girdle and shoulder girdle, and local tension in the anterior scalene muscle. Most often develops against the background of cervicothoracic osteochondrosis, abnormal cervical ribs, and trauma. Scalenus syndrome often occurs in adolescents who are intensely involved in sports (chronic injury to the anterior scalene muscle against the background of intensive skeletal growth and increased physical activity).
- Raynaud's syndrome. It is characterized by the localization of vegetative-vascular and trophic disorders mainly on the fingers and toes (pallor, cyanosis), as well as the suddenness and severity of attacks of vascular spasm, which become more and more protracted as the disease progresses. The leading factor in the development of the disease is compression and irritation of the arterial vessels of the arms and legs and the surrounding autonomic plexuses.
- Piriformis syndrome is a well-known SUD, in which there is compression of the sciatic nerve and inferior gluteal artery by the piriformis muscle in the buttock area. The clinical picture resembles “radiculitis” with pain spreading over the buttock and posterior thigh, limping, vegetative-vascular and neurodystrophic manifestations, as well as signs of local damage to the piriformis muscle, tension and pain of which can often be determined by touch.
— Carpal tunnel syndrome is the most common form of tunnel neuropathies. The median nerve is compressed in the carpal tunnel by the hypertrophied transverse ligament of the palm, which is clinically manifested by a sensation of “pins and needles” in the area of the hand and fingers, pain (especially when raising the arm up). With prolonged suffering, weakness of the hand muscles and trophic disorders develop. The prevalence of this syndrome has increased sharply due to total computerization, since computer keyboards turned out to be unsuitable for long-term work of the fingers with poor fixation of the wrists, which caused hypertrophy of the transverse carpal ligament and the occurrence of symptoms. This prompted computer companies to switch to special ergonomic keyboards, resulting in a sharp decline in the number of new cases of this rather unpleasant suffering.
To make an accurate diagnosis of NWS, both clinical studies (neurological examination using special functional tests) and numerous laboratory and instrumental methods are used to determine the state of the microcirculatory bloodstream, coagulation system and blood viscosity. Doppler ultrasound, electroneuromyography, capillaroscopy, computer thermal imaging, duplex scanning of blood vessels, and magnetic resonance imaging are also used. All these methods make it possible to accurately establish the localization and nature of muscular-tonic, vegetative-vascular and neurodystrophic disorders, to distinguish one form of SUD from another, and to select the correct treatment.
Therapy for these sufferings is divided into conservative and surgical. Conservative treatment is used for relatively early and benign current forms and is often very effective. It is aimed, first of all, at sources of neurovascular compression and vasospasm: spinal osteochondrosis, inflammatory and tumor processes of muscles and connective tissue, diseases of internal organs. The success of conservative treatment depends on the patient’s timely contact with a specialist. Self-medication is in any case unacceptable! Painkillers, drugs that improve microcirculation and relieve inflammation, decongestants and venotonic drugs are used.
Antispastic drugs (muscle relaxants) are important for treatment, since muscle spasm is not only a typical symptom, but also a key pathogenetic stage in the formation of almost any form of SUD. According to the experience of the most authoritative clinics in the world, the leading antispastic drug is currently recognized as baclofen (Baklosan), which not only effectively and quickly reduces muscle tone, but also has an undoubted analgesic effect. The latter circumstance is especially important in the treatment of SUD. Thus, the use of Baklosan and its analogues is an integral stage of therapy for NBC.
Blockades, acupuncture and electropuncture, electrical stimulation and other methods of physiotherapy, exercise therapy, massage, orthopedic and sanatorium treatment are also used in the treatment of SUD. If the disease has reached a severe stage, as well as if other methods of treatment are ineffective, surgical treatment is used (dissection of pathologically altered spasmodic muscles, removal of scar-fibrous deposits and ligaments, reconstructive operations on blood vessels).
© Magazine “Nerves”, 2006, No. 3
Medical Scientific and Practical Center for Vertebrology and Neuroorthopedics, Professor M.L. Kurganov
The names for this suffering are varied, just as its manifestations are varied. This syndrome was described in 1925 by doctors Barre and Lieu for cervical spondyloarthrosis. Now synonyms are often used: “posterior cervical sympathetic syndrome” , “cervical migraine” . Such diagnoses are often used in medical documentation and doctor's notes. Therefore, there is a need to explain to my patients what we are talking about. In a broad clinical sense, vertebral artery syndrome is a disturbance of blood flow to the brain in the basin of one or both vertebral arteries. A little about the blood supply to the head.
The brain is supplied with blood from 2 pools. The first - carotid - includes the carotid arteries. They (or rather, their main branches - the internal carotid arteries) provide up to 70-85% of blood flow and are responsible for all major circulatory disorders, primarily strokes. They are traditionally given special attention during examination; their atherosclerotic lesions and its complications are the object of special attention of cardiologists, neurologists, and vascular surgeons.
The vertebral arteries (right and left) belong to the vertebrobasilar region, supply blood to the posterior parts of the brain and, according to various sources, provide about 15-30% of blood flow. Their defeat does not lead to such serious complications as a stroke, but they can ruin the patient’s life for a long time and make him disabled.
Arterial damage manifests itself as
- severe dizziness,
- headache,
- loss of consciousness,
- coordination disorders,
- hearing and vision impairments.
The causes of damage to the vertebral arteries can be divided into 2 groups:
• The first group is non-vertebrogenic (not associated with the spine) lesions. They are caused either by atherosclerosis (it occurs much less frequently than in the carotid arteries), or by congenital anomalies in the size and course of the arteries. These anomalies usually have no independent significance, but when combined with other causes of arterial compression, they provide an unfavorable background.
• The second group is vertebrogenic (associated with spinal pathology) lesions. These are disorders caused by diseases of the spine. They can appear as early as adolescence with dysplastic and post-traumatic instability of the cervical spine. But the most pronounced changes develop in adults with the development of osteochondrosis.
The fact is that the artery passes part of its path to the skull in a bone canal formed by the transverse processes of the cervical vertebrae (starting from the 6th to the 1st vertebra). With osteochondrosis, deformation of the lateral (hook-shaped) processes of the vertebral bodies develops, the so-called uncovertebral arthrosis, and vertebral instability caused by the destruction of the intervertebral discs. All these reasons lead first to irritation of the sympathetic plexuses of the vertebral arteries, their subsequent spasm, and then to compression of the arteries throughout the entire bone canal or at the entrance and exit of the artery with the development of short-term circulatory disorders that occur when turning and tilting the head, changing position torso.
Clinical picture
The main characteristic symptom is headache . Characterized by a constant, sometimes intensifying, painful headache of a burning, sometimes pulsating nature in the occipital region. During an attack, pain can spread to other areas of the head, often radiating to the orbit and bridge of the nose (“cervical migraine”), to the parietal-temporal region, to the forehead, and ear. Most often localized on one side, it can be paroxysmal or permanent. The pain clearly intensifies with neck movements. Pain in the scalp often occurs even with a light touch or combing of the hair. When turning or tilting the head, a “crunch” is often heard, and sometimes a burning sensation is felt. In some patients, the syndrome manifests itself as dizziness with nausea or vomiting, a sensation of noise, ringing in the ears (often synchronous with the pulse). Dizziness develops when the head is raised upward (the artery goes into the narrow part of the hole), and with atherosclerosis of the cerebral vessels, dizziness develops when the head is tilted forward.
Sometimes there is decreased hearing and visual disturbances: decreased visual acuity, “spots”, blurred vision, fog before the eyes, double vision. Occasionally, swallowing problems and a sensation of a foreign body in the throat occur - the so-called pharyngeal migraine. When the vertebral artery is compressed, there are paroxysmal conditions that are clearly associated with turning the head:
- after turning the head, the patient falls “as if knocked down,” but does not lose consciousness, and soon gets up on his own;
- after a sudden movement of the head, the patient suddenly falls and loses consciousness. After 5 - 20 minutes he comes to his senses, gets up, but for a long time he feels weak.
There are also autonomic disorders: short-term feeling of hunger, thirst, feeling of heat or chills.
With a leading lesion of the sympathetic plexus of the vertebral artery, Bernard–Horner syndrome is noted. Pain and paresthesia in this case are often one-sided and can affect the face, hard palate, teeth, tongue, pharynx (tingling, burning, foreign body sensation). Vestibular disorders are usually observed in the form of spin, a feeling of staggering and sinking, accompanied by nausea, ringing and noise in the ear. During a headache, blurred vision, flashing before the eyes, increased fatigue, decreased performance, sweating, and chills may occur. In all cases there is a neurotic background. Changing the position of the head leads to increased headaches, but the patient can find a certain position in which the pain disappears or decreases.
Diagnostics and additional methods
Currently, the main method for diagnosing circulatory disorders in the vessels supplying the brain is generally accepted to be Doppler ultrasound (USD).
The study of the arteries of the carotid and vertebrobasilar basins is called USDG of the branches of the aortic arch or USDG of estracranial vessels. However, when performing a standard ultrasound examination, the main attention is traditionally paid to the carotid arteries, and the examination of the vertebral arteries is performed only partially. This is also due to the lack of uniform standards and differences between different schools of specialists. Often the artery is not examined along its entire length, but only in the initial and final segments, functional tests are not performed, the conclusion about the pathology of the vertebral arteries is made based on indirect data, the specific causes and level of compression are not indicated.
Treatment of vertebral artery syndrome: When treating this condition, the main goal is adequate blood circulation in the vertebral arteries , as well as eliminating or minimizing the causes of irritation or vascular spasm. The treatment uses methods of manual therapy, reflexology, vacuum therapy, pharmacopuncture, magnetic therapy, exogenous bioresonance therapy with fixed frequencies. Vascular therapy is necessarily involved in the complex of therapeutic measures. If necessary, anti-inflammatory drugs and mild antidepressants are prescribed.
Vertebral artery syndrome
Analysis of literature data has shown that currently there is no unambiguous definition and unified classification of vertebral artery syndrome (VA), this allows this diagnosis to determine various pathologies - posterior cervical sympathetic syndrome (Barre-Lieu syndrome, cervical migraine, spinal nerve lesion syndrome), vertebrogenic cervicocranialgia or use the general term - vertebrobasilar insufficiency and/or chronic cerebral ischemia. In the review part of this article, an attempt was made to clarify the concept of the term and classification of PA syndrome. At the same time, new possibilities for pathogenetic therapy and improving the patient’s quality of life are also considered.
The basis of VSPA in the examined patients was vertebrogenic compression and irritation of the sympathetic plexus of the vertebral artery, most often in the V2 segment, against the background of uncovertebral growths (55.5% of cases) and instability of the cervical spine (16.7%), as well as in the V3 segment against the background of muscular-tonic tension of the inferior oblique muscle of the capitis (14.8%) and pathology of the craniovertebral junction (9.3%). VBI syndrome occurred in patients with vertebrogenic pathology of the cervical spine (100%) in combination with long-term arterial hypertension (81%) and cerebral atherosclerosis (76%).
The International Classification of Diseases, 10th revision (ICD-10) indicates several diagnoses characterizing damage to the vertebrobasilar bed: M.47.0 - VA compression syndrome in spondylosis (VA syndrome); M.53.0 - cervicocranial syndrome (posterior cervical sympathetic syndrome); G.45.0—vertebrobasilar arterial system syndrome [18, 19, 27]. The diagnosis of VA syndrome is usually made when a vertebrogenic variant of VA compression is suspected [26]. If the VA is directly exposed to vertebrogenic influence, we are talking about a compression variant of the VA syndrome, which is of key importance in the presence of atherosclerosis of the arteries of the vertebrobasilar system, especially bilateral, when the possibility of collateral blood flow is practically excluded, and the vertebrobasilar arterial system syndrome occurs. In this case, they speak of vertebrobasilar insufficiency and/or cerebrovascular accident in the vertebrobasilar arterial system [4, 20, 22, 23]. If the fibers of the sympathetic plexus surrounding the VA are subjected to compression, then this means an irritative variant of the VA syndrome with the occurrence of vascular spasm not only in the VA that is directly subjected to compression, but also in the opposite VA and in the arteries of the overlying carotid system. The irritative type of PA syndrome is usually observed in young patients who do not have concomitant pathology of the vertebrobasilar bed. In people of the older age group, the most common mixed compression-irritative variant of PA syndrome occurs. In addition, VA spasm can develop as a result of a reflex response to irritation of the afferent structures of the affected spinal motion segment of the cervical spine. In this case, PA syndrome is designated as reflex-angiospastic, the degree of clinical manifestation of which almost always remains mild or moderate. However, it should be noted that in some cases it is minor chronic irritation of the vertebral nerve and the periarterial sympathetic plexus of the VA that leads to pronounced changes in the tone of the brachiocephalic and cardiac vessels, and dystrophic changes in the myocardium and neck muscles. This feature is important because many authors in their works focus on severe, easily identified compression factors, underestimating the role of muscle and reflex mechanisms [5].
Thus, PA syndrome is a collective concept that unites a complex of cerebral, vascular, autonomic syndromes that arise as a result of damage to the sympathetic plexus of the PA, deformation of its wall or changes in the lumen [6]. The prevalence of PA syndrome in degenerative-dystrophic manifestations of cervical spine pathology is 30.0–42.5% [11].
In the historical aspect, the first descriptions of the close relationship of the cervical spine, VA and the surrounding sympathetic plexus date back to 1925, when M. Wagge [15] described an unusual type of headache combined with visual, auditory, vestibular and autonomic disorders in patients with osteochondrosis and spondylosis of the cervical spine. Subsequently, his student Y. Lieou called this symptom complex posterior cervical sympathetic syndrome. W. Bartschi-Rochain, studying traumatic injuries of the cervical spine, used the term “cervical migraine” [16]. Note that this term is rarely used in Russian neurology, although it is used by many both foreign and domestic authors [3, 24, 25].
Currently, there are numerous additional methods for examining the patient (radiography of the cervical spine with functional tests, radiography of the craniovertebral junction, duplex scanning of the brachiocephalic arteries, arteries of the circle of Willis, magnetic resonance and X-ray computed tomography of the cervical spine, etc.), which help in the diagnosis diagnosis of PA syndrome. However, despite the available possibilities, accurate diagnosis of PA syndrome is often difficult, since this condition does not always meet clear clinical diagnostic criteria and requires long-term observation of the patient with the development of an individual plan for his examination and treatment.
The topographic-anatomical location of the VA in a narrow mobile bone canal formed by the transverse processes of the cervical vertebrae creates the possibility of its injury. PA penetrates into this canal through a hole in the transverse process of the CVI vertebra, less commonly the CVII, CV or CIV vertebrae. In this channel, the PA is accompanied by a dense sympathetic nerve plexus, which is connected with the cervical sympathetic ganglia, including the stellate ganglion (cervicothoracic ganglion, gangl. stellatum), which provide innervation not only to the vertebrobasilar region, but also send branches to the heart , larynx, etc. In addition, numerous recurrent branches extend from the sympathetic plexus to the vertebrae, joints and intervertebral discs. Having passed through CI, the PA is located in the groove on the posterior arch of the atlas, where it is covered almost exclusively by one inferior oblique muscle of the head and then penetrates into the cranial cavity through the foramen magnum. Considering the described anatomical features of PA, it is easy to assume that even minor degenerative-dystrophic changes in the cervical spine can lead to the occurrence of PA syndrome. Of great importance in the formation of PA syndrome are hyperexthetic injuries of the cervical spine, especially with rotation of the cervical spine - “whiplash injury” with the emergence of a characteristic clinical picture of PA syndrome in both acute and long-term periods [8, 19] . Chronic irritation of the sympathetic plexus has been well studied in cervical spondylosis [27], uncovertebral arthrosis, posterolateral disc herniations, instability of the motor segments of the cervical spine, various anomalies of the craniovertebral junction, congenital blocks of the cervical spine, hypoplasia and/or congenital or acquired pathological tortuosity of the VA, after manual manipulation of the cervical spine, especially when there are pronounced degenerative changes and other pathology of the cervical spine [2, 10, 28].
It is known that the mediator of the sympathetic nervous system is norepinephrine, which is contained in the endings of sympathetic fibers. Norepinephrine is a precursor of adrenaline, but differs from it by a much more powerful vasoconstrictor and pressor effect. Norepinephrine takes part in the regulation of blood pressure and peripheral vascular resistance, has an activating effect on the reticular formation; it is the most important mediator of wakefulness. The action of norepinephrine is associated with a predominant effect on α-adrenergic receptors. The cardiotropic effect of norepinephrine is associated with its stimulating effect on β-adrenergic receptors of the heart [1, 9]. Long-term disruption of vascular innervation due to cervical osteochondrosis can lead to persistent changes in blood pressure, when even etiotropic therapy does not provide improvement. This is due to the fact that a vicious circle arises: osteophytes of the cervical vertebrae cause compression of the VA and irritation of its sympathetic plexus. Under certain conditions, thanks to anatomical connections, the branches of the internal carotid artery are also involved in the process, and irritation aggravates vascular spasm. As a result, ischemia and inadequate functioning of the hypothalamic region occur, which is aggravated by repercussive changes in the hypothalamus due to irritation of the sympathetic plexus of the VA [13, 14, 27].
Clinical manifestations of PA syndrome depend on the causes that caused this condition. Post-traumatic PA syndrome has a greater severity of neurological symptoms and a clear clinical picture. Chronic irritation of the surrounding sympathetic plexus, as mentioned above, leads to persistent tone of the brachiocephalic and cranial arteries and is manifested by cerebrovascular disorders of varying degrees. Concomitant diseases, such as atherosclerosis of the brachiocephalic arteries, brain, hypertension, coronary heart disease, or a combination thereof, are also of great importance in the symptom complex of PA syndrome. It should be noted that patients with chronic vertebrobasilar insufficiency caused by vascular and extravascular factors also experience episodes of PA syndrome, which is usually verified as an exacerbation of vertebrobasilar insufficiency. In this regard, for an accurate diagnosis, anamnestic data should be taken into account, especially the events that immediately preceded the development of PA syndrome - discoordinated movements in everyday life (reaching for water, getting something from the top shelf, etc.) or when playing sports, long-term stay in a static position (working with the head thrown back up, reading in a position of deep flexion and/or rotation of the neck, hyperextension of the cervical spine during tooth traction), sleeping in an unusual place (at a party, on a newly purchased sofa), performing manual manipulations .
The most common clinical variants of PA syndrome are: posterior cervical sympathetic syndrome—a unique symptom complex regarded as a functional stage of PA syndrome [7]. It is characterized by a headache in the cervico-occipital region of a pulsating or burning nature with irradiation to the anterior parts of the head and the periorbital region, accompanied, in some cases, by lacrimation, nasal congestion and other vegetative manifestations. Headache with this syndrome can be constant, especially in the morning after sleeping on an uncomfortable pillow, when walking, shaking, or when moving the neck [11]; vestibulo-atactic syndrome - most often accompanies headache (subjective symptoms predominate: dizziness, a feeling of body instability, darkening of the eyes, imbalance with nausea and vomiting, cardiovascular disorders [10, 12, 17]; cochleo-vestibular syndrome; ophthalmic syndrome; syndrome of autonomic disorders (up to severe hypothalamic crises).
In severe cases of the disease, transient circulatory disorders in the vertebrobasilar system, drop attacks, and syncope develop [4].
Summarizing the above, we can highlight the characteristic features of PA syndrome in terms of its difference from other vascular syndromes. PA syndrome develops as a result of vertebrogenic effects on the sympathetic nerve plexus of the PA and/or direct compression of the PA and is manifested by characteristic clinical symptoms associated primarily with the release of norepinephrine into the systemic bloodstream, which, by binding to vascular α-adrenergic receptors, has a systemic and peripheral vasospastic effect. The severity of symptoms varies from mild (headache, dizziness, slight increases in blood pressure) to significant (severe hypothalamic crises and/or a sharp simultaneous increase in blood pressure) and depends on the etiopathogenetic factor that caused this condition.
This work was carried out taking into account existing ideas about the etiology and mechanism of development of PA syndrome and the direct participation of adrenergic mechanisms in the development of symptoms. Its purpose was to evaluate the effectiveness of the drug sermion (nicergoline) in patients with PA syndrome.
The drug sermion is a derivative of ergot and is currently used in more than 50 countries around the world [21]. Nicergoline contains an ergoline core and a bromine-substituted nicotinic acid residue and exhibits an adrenergic blocking effect [29]. It is the adrenergic blocking effect that determines its pharmacotherapeutic effectiveness in PA syndrome. This effect significantly distinguishes sermion from other vascular drugs, the vasodilating effect of which is carried out using other mechanisms. The prescription of drugs that do not have an -adrenergic blocking effect has a symptomatic, but not pathogenetic orientation, gives good results, and can be indicated in cases of poor tolerability of nicergoline. However, it should be borne in mind that the effect of symptomatic therapy is less long-lasting. The duration of therapy with Sermion is determined by the degree of improvement in the patient’s clinical condition and averages from 3 to 6-12 months.
Bibliography:
- Ashmarin I.P., Eshchenko N.D., Karazeeva E.P. Neurochemistry in tables and diagrams. M: Exam 2007; 27-30.
- Bragina L.K., Kozlova E.N. The significance of vertebral artery hypoplasia in the pathogenesis of cerebrovascular accident. J. Neuropath and Psychiat 1979; 79:9:1329-1332.
- Vereshchagin N.V. Damage to the extracranial parts of the vertebral arteries and cerebrovascular accidents: Abstract of thesis. dis. ...cand. honey. Sci. M 1964; 6-12.
- Vereshchagin N.V. Pathology of the vertebrobasilar system and cerebrovascular accidents. M: Medicine 1980; 420.
- Zhulev N.M. et al. Vertebral artery syndrome. St. Petersburg 2001; 224.
- Kalashnikov V.I. Vertebral artery syndrome. Therapia 2007; 10: 31-33.
- Kalashnikov V.I. Vertebral artery syndrome: clinical variants, classification, principles of diagnosis and treatment. Practicing neurologist. To Practicing Neurologist 2010; 1:31:93-99.
- Kozlov M.Yu. Diagnosis and treatment of cervical whiplash injury. Neurology and Neurosurgery 2003; 3: 17-28.
- Nicholls J., Martin A., Wallas B., Fuchs P. From neuron to brain: Trans. from English Ed. 2nd. M: LKI Publishing House 2008; 117-121.
- Petryanina E.L., Ismagilov M.F. Vertebral artery syndrome caused by an abnormal structure of the cervical spine. Neurological Bulletin 1994; XXVI: 3-4: 58-59.
- Popelyansky Ya.Yu. Diseases of the peripheral nervous system: A guide for doctors. M: Medicine 1989; 315-463.
- Pyshkina L.I., Fedin A.I., Besaev R.K. Cerebral blood flow in vertebral artery syndrome. J. Neuropathol and Psychiat 2000; 5:45-49.
- Ratner A.Yu. Cervical osteochondrosis and cerebral disorders. Kazan: Kazan University Publishing House 1970; 231.
- Yunonin I.E., Khrustalev O.A., Kurapin E.V., Yunonina L.V. Arterial hypertension and cervical osteochondrosis of the spine. Ros Cardiol Journal 2003; 4: 88-94.
- Barre JA Sur un syndrome sympathique cervical posterieur et sa cause fryquonte: L'arthrite cervical. Rev neurol 1926; 33:1:1246-1248.
- Bartscbi-Rocbaix W. Migraine cervicale. Bern 1949; 9-12.
- Berguer R., Flynn LM, Kline RA, Caplan L. Surgical reconstruction on the extracranial vertebral artery: management and outcome. J Vasc Surg 2000; 31:9-18.
- Davis RV Therapeutic Modalities for the Clinical Health Sciences, 2nd, 1989. Library of Congress Card TXU 389 661.
- Davis RV Management of Vertebral Artery Syndrome. Dynamic Chiropractic 1994; 12: Issue 17.
- Draper R. Vertebrobasilar Occlusion and Vertebral Artery Syndrome. EMIS 2009. Document ID: 1701. Version: 21.
- Fioravanti M., Flicker L. Efficacy of nicergoline in dementia and other age associated forms of cognitive impairment. Cochrane Database Syst Rev 2001; 4: CD003159.
- Kaye V. Vertebrobasilar Stroke Overview of Vertebrobasilar Stroke. Eur J Neurol 2006; 13: 4: 395-401.
- Kumral E., Kisabay A., Ataç C. Lesion patterns and etiology of ischemia in the anterior inferior cerebellar artery territory involvement: a clinical — diffusion weighted — MRI study. Eur J Neurol 2006; 13:4:395-401.
- Kunert W. Arteria vertebralis und Halswirbelsaule. Stuttgart 1961; 5065.
- Meyer IS Occlusive cerebrovascular disease. Pathogenesis and treatment. Amer J Med 1961; 4: 30: 577-588.
- Powers SR, Drislane TM, Nevins S. Intermittent vertebral artery compression. A new syndrome. Surgery 1961; 49: 257-264.
- Watanuki A. The effect of the sympathetic nervous system on cervical spondylosis. Nihon Seikeigeka Gakkai Zasshi 1981; 55:4:371-385.
- Williams D. Vertebro-basilar Ischaemia. Br Med J 1964; 1:5375:6-84.
- Winbland B. Therapeutic use of Nicergoline. Clin Drug Investigation 2008; 28:9.
Taken from the site